Airway Assessment
Published (updated: ).
When the patient is alert and talking to you, the airway is clear.
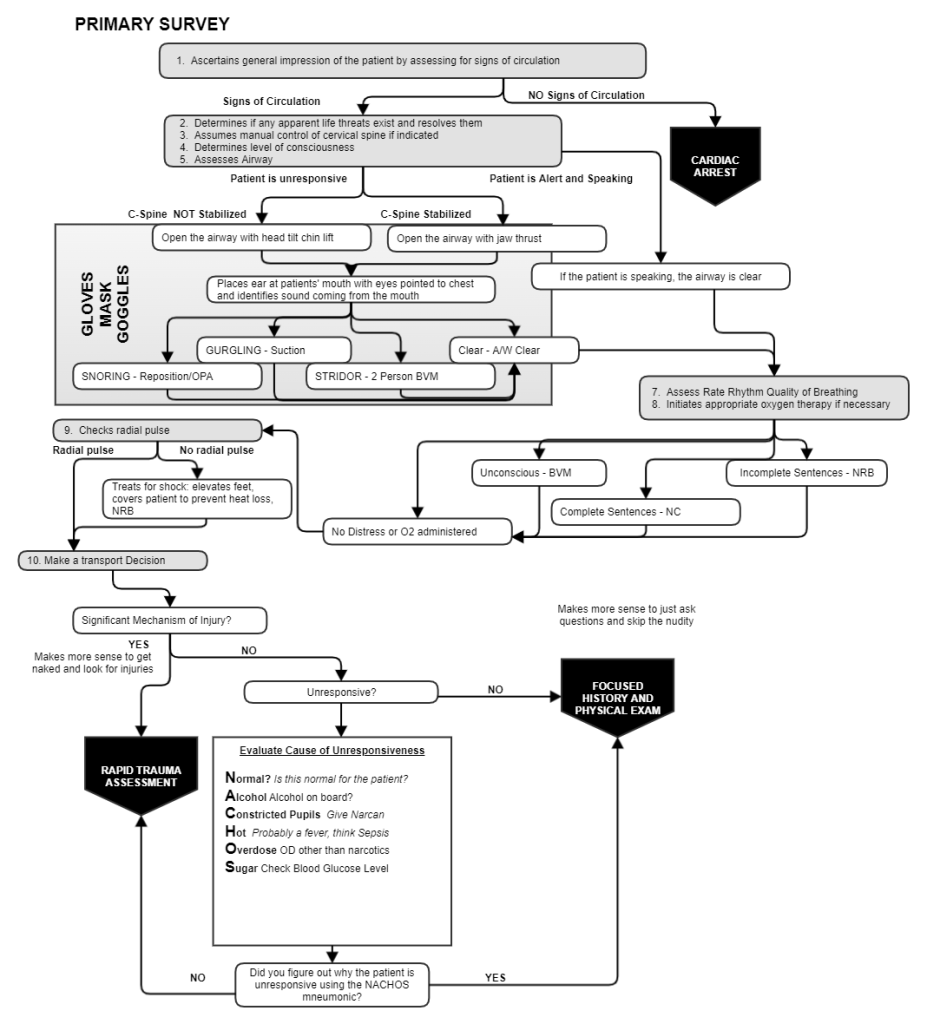
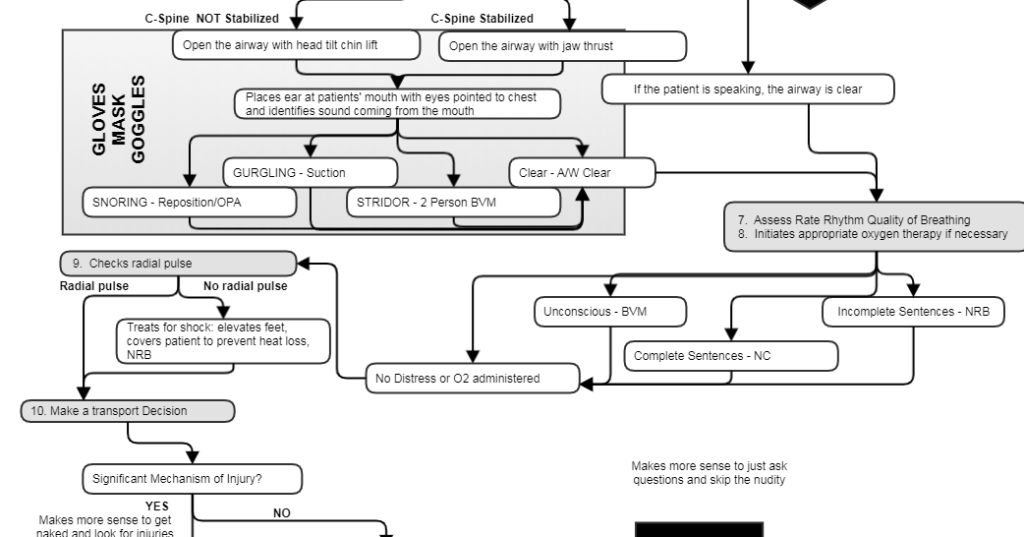
When the patient is not alert and is not speaking to you, the airway must be assessed
In a patient who is unresponsive or not alert, the cause of the altered mental status could be an airway obstruction of some sort, so we have to assess the airway. If the airway is obstructed, the patient will be unable to talk or breath. If the airway is obstructed, there will be little or no air passing through the patient’s mouth. If the airway is partially obstructed, then the sounds coming out of the patient’s mouth when the breath (or attempt to breath) will be noisy.
To assess the airway, one must look for evidence that it is obstructed.
You can open the airway like you open a door.
To assess and airway on a patient who is breathing, the rescuer needs to open the airway, then place their ear at the patient’s mouth while looking at the chest observing for chest rise. If the chest is rising and clear sounds are heard from the mouth, then the airway is clear. If the chest is rising and the sounds coming from the mouth are noisy, then there is a partial obstruction. The sounds that could be heard are:
- Gurgling sounds – Indicate fluids in the mouth
- Snoring – The sound made when the tongue obstructs the airway
- Stridor – Screeching or high pitched sound coming out of the mouth is made when air is passing through an airway that is constricted (or smaller) due to an obstruction.
Things that can obstruct the airway are:
- Tongue
- Food
- Vomit
- Blood
- Teeth
- Foreign body (like a toy or coin)
- Swelling due to trauma (usually burns) or infection (which would cause swelling to the vocal cords)
