The Mechanics of Maintaining Adequate Blood Pressure Even In Times of Peril
Published (updated: ).
When the patient experiences a drop in blood pressure due decreased cardiac output the body unleashes a host of compensatory mechanisms. Human beings are constantly moving and changing positions. Increased workload of the body requires a circulatory system that is dynamic enough to maintain blood pressure in all situations. Usually, these countermeasures ensure consistent and adequate blood pressure for all the years of a patients’ life. Sometimes, a patient will have a problem that is just too big for the compensatory mechanisms of the circulatory system to resolve. Further, these compensatory mechanisms were designed to be temporary measures; after some time the effectiveness of these measures will drop and even be counterproductive.
Circulating catecholamines, epinephrine and norepinephrine, originate from two sources. Epinephrine is released by the adrenal medulla upon activation of preganglionic sympathetic nerves innervating this tissue. This activation occurs during times of stress (e.g., exercise, heart failure, hemorrhage, emotional stress or excitement, pain). Norepinephrine is also released by the adrenal medulla. Normally, most of the norepinephrine released by sympathetic nerves is taken back up by the nerves (a small fraction is also taken up by extra-neuronal tissues) where it is metabolized. A small amount of norepinephrine that is recycled and metabolized diffuses into the blood and circulates throughout the body. At times of high sympathetic nerve activation, the amount of norepinephrine entering the blood increases dramatically.
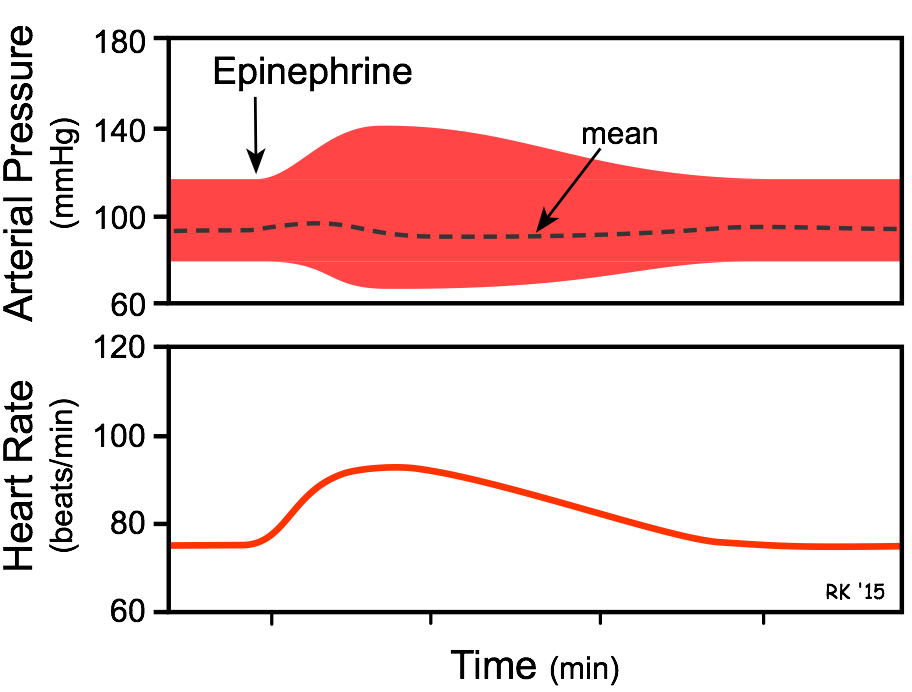
Circulating Epinephrine Effects:
- Increased heart rate and cardiac contractile force
- Vasoconstriction in most systemic arteries and veins.
- Vasodilation in muscle and liver vasculatures at low concentrations; vasoconstriction at high concentrations.
- The overall cardiovascular response to low-to-moderate circulating concentrations of epinephrine is increased cardiac output and a redistribution of the cardiac output to muscular and hepatic circulations with only a small change in mean arterial pressure.
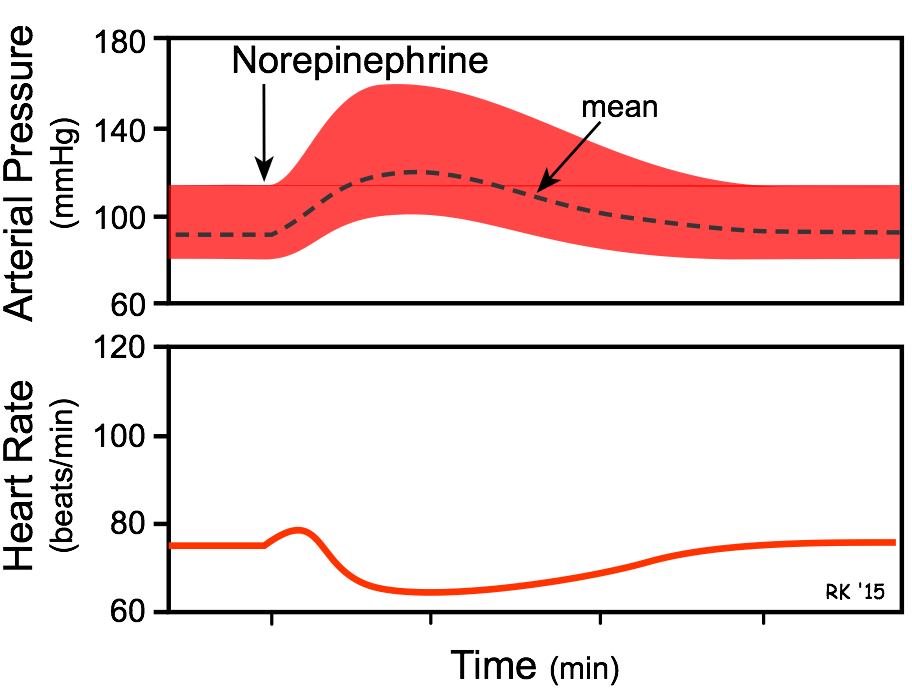
Circulating Norepinephrine Effects:
Increased heart rate (although only transient) and increased cardiac contractile force are the direct effects norepinephrine on the heart. Vasoconstriction occurs in most systemic arteries and veins.
The overall cardiovascular response is increased cardiac output and systemic vascular resistance, which results in an elevation in arterial blood pressure. Heart rate, although initially stimulated by norepinephrine, decreases due to activation of baroreceptors and vagal-mediated slowing of the heart rate in responses to the elevation in arterial pressure.
Long story short, when the brain senses a drop in arterial pressure, it signals the adrenal glands to secrete epinephrine and norepinephrine which increases cardiac output by increasing heart rate and contractile force. Epinephrine also makes the vascular system smaller by contracting which results in a higher blood pressure.
