How People Die: Respiratory Failure
Published (updated: ).
When a patient’s respiratory system becomes compromised, the patient is very close to death. If the patient doesn’t improve, the next step is death. Any condition or injury that affects breathing can cause respiratory failure. The condition or injury may affect the airway or lungs. Or it may affect the muscles, nerves, and bones that make breathing possible. When a patient isn’t breathing well, their lungs can’t easily move oxygen into the blood or remove carbon dioxide. This causes a low oxygen or high carbon dioxide level in your blood.
Respiratory failure can be caused by:
- Conditions that make it difficult to breathe in and get air into the lungs. Examples include weakness following a stroke, collapsed airways, and food getting stuck in and blocking your windpipe.
- Conditions that make it difficult for exhale. Asthma causes your airways to narrow, while COPD can cause mucus to buildup and narrow the lower airways, which can make it hard exhale.
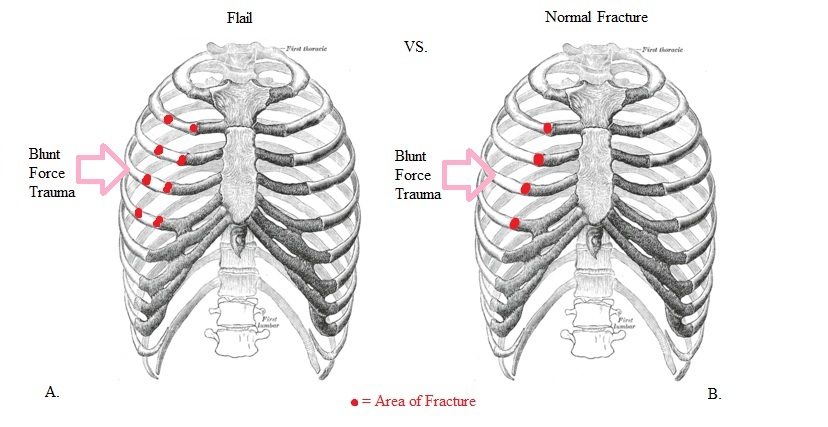
- Lung collapse. When no air is able to enter the lungs, one or both lobes may collapse and cause a condition called atelectasis. This collapsing of the lung can happen in certain situations, such as when the lungs become extremely weak, mucus blocks one of the large airways, a rib is broken or fractured, or severe pain in the lung makes it difficult to take a deep breath. Chest trauma or lung injury can also cause air to leak from the lung, filling the space around the lung within the chest. This air could cause the lung to collapse, called a pneumothorax.
- Fluid in the lungs. This makes it harder for oxygen to pass from the air sacs into your blood and for carbon dioxide in the blood to pass into the air sacs to be breathed out. Pneumonia, acute respiratory distress syndrome (ARDS), drowning, and other lung diseases can cause this fluid buildup. It can also be caused by the inability of the heart to pump enough blood to the lungs (called heart failure). Severe head injury or trauma can also cause sudden fluid buildup in the lungs.
- A problem with muscles of respiration. Such problems can occur after a spinal cord injury or when you have a nerve and muscle condition such as muscular dystrophy. It can also happen when the diaphragm and other breathing muscles do not get enough oxygen-rich blood, when the heart is not pumping well enough (cardiogenic shock), or when the patient has sepsis.
- Conditions that affect the brain’s control over breathing. In opioid overdose, for example, the brain may not detect high levels of carbon dioxide in the blood. Normally, the brain would signal the lungs to deepen your breathing so that you breathe out the carbon dioxide. Instead carbon dioxide builds up in the body, while oxygen levels fall, leading to respiratory failure.
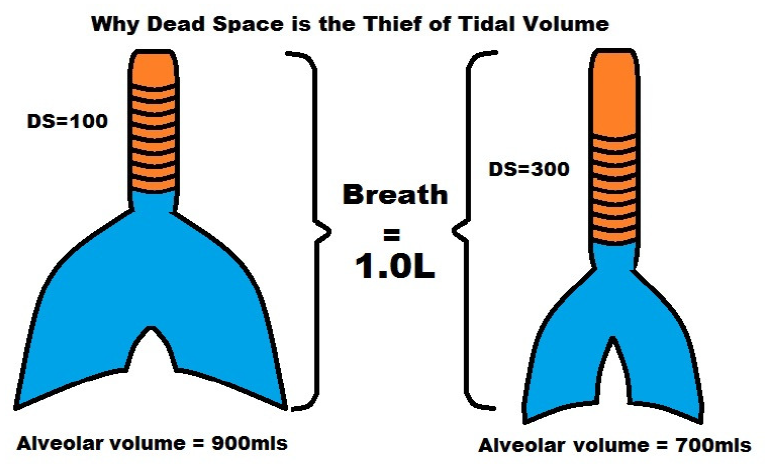
Tidal volume is the amount of air that travels into the lungs with a given breath. Let’s say that the patient is breathing 1 liter with each breath. Assuming the patient was breathing 12 times a minute, the minute volume would be 12 liters. Each breath has double duty, it has to fill the dead space with air before any air reaches the alveoli. In this example, the dead space was measured to be 300 ml. Alveolar volume would be measured by substracting the dead space (300 ml) from the tidal volume (700 ml).
From this understanding the medic could determine if the patient was not breathing adequately and needed ventilatory assistance (positive pressure ventilation). Minute Alveolar Ventilation is the amount of air actually reaching the alveoli (which is where the gas exchange occurs). If the patient from the above scenario was only breathing 4 times a minute (probably due to a narcotic overdose), and still possessed the same dead space of 300 ml resulting in a alveolar ventilation volume of 700 and a minute alveolar ventilation volume of 2800, the patient would not be moving enough air to the alveoli to meet the oxygen demands of the patient’s body. The same dynamics would apply if the patient was breathing 12 times a minute but only moving 500 ml of air instead of 1 liter. Subtracting the dead space of 300 ml is going to result in a minute alveolar ventilation volume of 2400 ml, also significantly less than the patient requires.
In both cases the patient needs ventilatory assistance in the form of positive pressure ventilation. In both cases, the patient will more than likely be unconscious (who else would you bag?).
