More Threats To Perfusion
Published .
Ventilation To Perfusion (Q/V) Mismatch
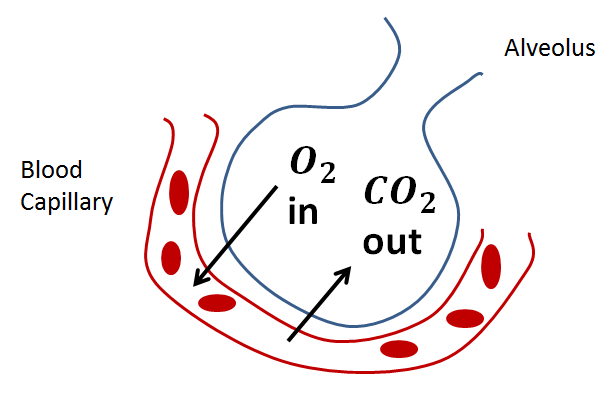
One of the major roles of the lungs is to facilitate gas exchange between the circulatory system and the external environment. The lungs are composed of branching airways that terminate in respiratory bronchioles and alveoli, which participate in gas exchange. Most bronchioles and large airways are part of the conducting zone of the lung, which delivers gas to sites of gas exchange, in alveoli. Gas exchange occurs in the lungs between alveolar air and blood of the pulmonary capillaries. For effective gas exchange to occur, alveoli must be ventilated and perfused. Ventilation (V) refers to the flow of air into and out of the alveoli, while perfusion (Q) refers to the flow of blood to alveolar capillaries.
Gas exchange in the alveoli occurs primarily by diffusion. Traveling from the alveoli to capillary blood, gases must pass through alveolar surfactant, alveolar epithelium, basement membrane, and capillary endothelium. According to Fick’s law of diffusion, diffusion of a gas across the alveolar membrane increases with:
- Increased surface area of the membrane
- Increased alveolar pressure difference (PA-Pa)
- Increased solubility of the gas
- Decreased membrane thickness
Mechanism
The V/Q ratio evaluates the matching of ventilation (V) to perfusion (Q). Systemic circulation to the lungs takes place via the bronchial circulation, which ultimately drains into the pulmonary vein. Physiological conditions can cause extreme V/Q ratios outside of the normal range. Generally, increasing FiO2 through supplemental oxygen therapy does not improve hypoxemia in patients with V/Q midmatch. The increased oxygen content of the inspired air never reaches the shunted blood for gas exchange.
Alveolar dead space occurs when some alveoli are not ventilated, resulting in a low V/Q ratio. Alveolar dead space increases the total physiological dead space, decreasing alveolar ventilation; this results in a decreased V/Q ratio and decreases PAO2 for functional alveoli.
Clinical Significance
A number of conditions can cause a V/Q mismatch. Congenital heart defects, ventricular septal defects. airway obstructions, pulmonary edema, and pneumonia. Asthma is often referred to as a “false shunt” because bronchoconstriction decreases ventilation, resulting in a low V/Q ratio, as occurs in alveolar dead space. In the case of asthma, oxygen therapy is indicated because some ventilation of the bronchoconstricted alveoli still occurs, and oxygen therapy increases the oxygenation of alveoli with obstructed airflow. Treatment with a bronchodilator such as a beta-2 agonist is more beneficial to patients with asthma than oxygen therapy because of its reduction of bronchoconstriction.
V/Q mismatches can occur in the case of pulmonary embolism (PE). Emboli may restrict blood flow in the pulmonary circulation, resulting in alveoli that are ventilated but not perfused; this results in an increased V/Q ratio and decreased gas exchange. The impaired gas exchange may cause hypoxemia.
Inspiratory hypoxia, as occurs at high altitude, can cause a V/Q mismatch and affect blood gases. The decreased atmospheric pressure at altitude causes a decreased PAO2. Although normal diffusion occurs (normal A-a gradient), the arterial PaO2 decreases and hypoxemia results. Oxygen therapy can correct the hypoxemia in this instance because the inspired air increases the PAO2 back to normal levels.
A significant cause of diffusion problems is pulmonary edema, as fluid in the lungs increases the effective thickness of the alveolar wall and decreases the area of gas exchange. Pulmonary edema results in greater hypoxemia than hypercapnia because carbon dioxide can more easily dissolve into the fluid to reach the alveolar membrane for exchange. The edema prevents air from reaching pulmonary capillaries, resulting in perfusion without ventilation and alveolar dead space.
