More Tissue & Cell Exchange
Published (updated: ).
Blood Reservoir
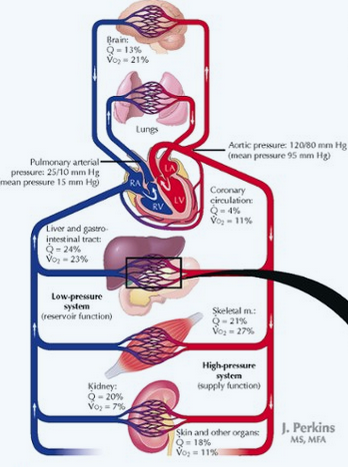
More than 60 per cent of all the blood in the circulatory system is usually in the veins. For this reason and also because the veins are so compliant, it is said that the venous system serves as a blood reservoir for the circulation.
When blood is lost from the body and the arterial pressure begins to fall, nervous signals are elicited from the carotid sinuses and other pressure-sensitive areas of the circulation. These in turn elicit nerve signals from the brain and spinal cord mainly through sympathetic nerves to the veins, causing them to constrict. This takes up much of the slack in the circulatory system caused by the lost blood. Indeed, even after as much as 20 per cent of the total blood volume has been lost, the circulatory system often functions almost normally because of this variable reservoir function of the veins.
Specific Blood Reservoirs. Certain portions of the circulatory system are so extensive and/or so compliant that they are called “specific blood reservoirs.” These include
- The spleen, which sometimes can decrease in size sufficiently to release as much as 100 milliliters of blood into other areas of the circulation
- The liver, the sinuses of which can release several hundred milliliters of blood into the remainder of the circulation.
- The large abdominal veins, which can contribute as much as 300 milliliters.
- The venous plexus beneath the skin, which also can contribute several hundred milliliters. The heart and the lungs, although not parts of the systemic venous reservoir system, must also be considered blood reservoirs. The heart, for instance, shrinks during sympathetic stimulation and in this way can contribute some 50 to 100 milliliters of blood; the lungs can contribute another 100 to 200 milliliters when the pulmonary pressures decrease to low values.
Maintaining pH

The process of perfusion which also includes breaking down carbohydrates, fats, and proteins produces results in the accumulation of hydrogen molecules. Chemically speaking, hydrogen bonds with everything to form all sorts of different compounds. Hydrogen is the consistent ingredient in acids. Since the human the body is 60% water (much of it in the blood), the pH must be regulated very carefully (like a very diligent pool boy).
The blood offers multiple methods of pH maintenance. The kidneys produce and recycle bicarbonate. Bicarbonate is released into the bloodstream in the kidneys which serves to raise the pH. Protein in blood plasma also act as a buffering agent. Hemoglobin (which is protein based) also acts as a buffer. There are other buffering agents in play as well. These methods must keep the pH within a normal range (pH 7.35 – 7.45) or risk the destabilization of cell membranes.
Infection Response
The immune system includes certain types of white blood cells. It also includes chemicals and proteins in the blood, such as antibodies, complement proteins, and interferon. Some of these directly attack foreign substances in the body, and others work together to help the immune system cells.
Lymphocytes are a type of white blood cell. There are B and T type lymphocytes.
- B lymphocytes become cells that produce antibodies. Antibodies attach to a specific antigen and make it easier for the immune cells to destroy the antigen.
- T lymphocytes attack antigens directly and help control the immune response. They also release chemicals, known as cytokines, which control the entire immune response.
As lymphocytes develop, they normally learn to tell the difference between your own body tissues and substances that are not normally found in your body. Once B cells and T cells are formed, a few of those cells will multiply and provide “memory” for your immune system. This allows your immune system to respond faster and more efficiently the next time you are exposed to the same antigen. In many cases, it will prevent you from getting sick. For example, a person who has had chickenpox or has been immunized against chickenpox is immune from getting chickenpox again.
Coagulation
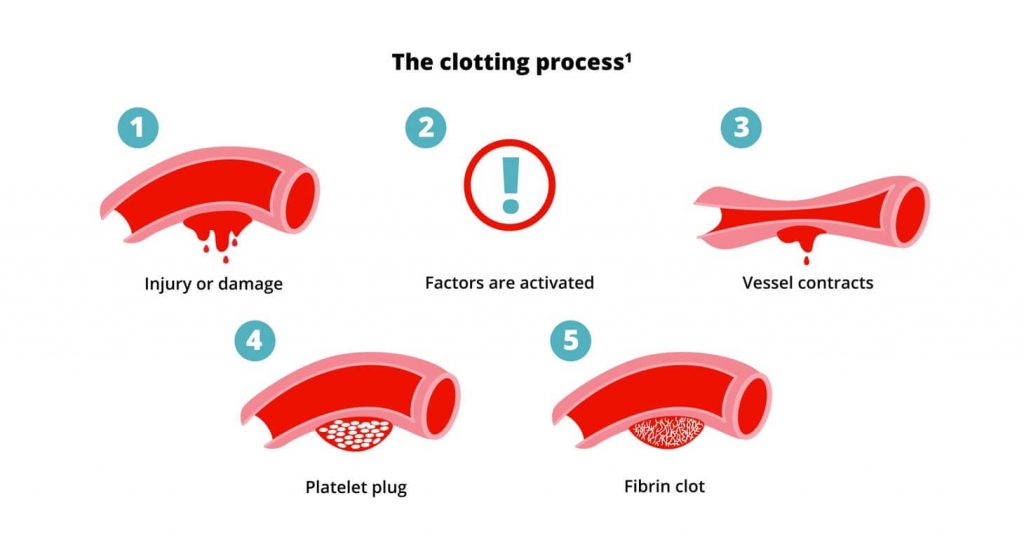
Clotting factors are proteins found in blood that work together to make a blood clot. They are designated by Roman numerals I through XIII.
Blood vessels shrink so that less blood will leak out. Tiny cells in the blood called platelets stick together around the wound to patch the leak. Blood proteins and platelets come together and form what is known as a fibrin clot. The clot acts like a mesh to stop the bleeding.
Bleeding causes a biological “domino effect” in which a series of steps are set in motion. When your body detects a bleed, the clotting factors are switched on in a particular order, one after the other.
Each factor activates the next until they form a clot. This is known as the coagulation cascade. Intrinsic and extrinsic pathways are 2 separate pathways that lead to the formation of a clot. The intrinsic pathway is activated early in the coagulation cascade, known as the initiation phase. The extrinsic pathway activates during the amplification phase of the coagulation cascade—increasing the number of platelets at the site of a bleed.
When certain blood-clotting factors are deficient or missing in a person with a bleeding disorder, the blood does not clot as it should, and it takes longer for a clot to form and for bleeding to stop.
