Advanced Directives
Published (updated: ).
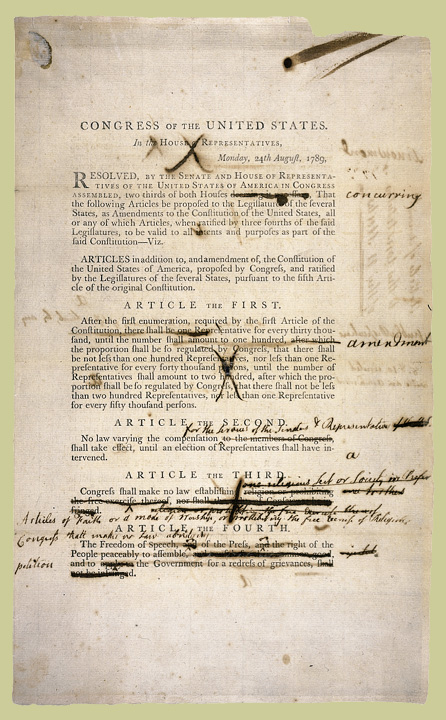
The Constitution of the United States of America is the supreme law of the United States. Empowered with the sovereign authority of the people by the framers and the consent of the legislatures of the states, it is the source of all government powers, and also provides important limitations on the government that protect the fundamental rights of United States citizens.
The need for the Constitution grew out of problems with the Articles of Confederation, which established a “firm league of friendship” between the states, and vested most power in a Congress of the Confederation. This power was, however, extremely limited — the central government conducted diplomacy and made war, set weights and measures, and was the final arbiter of disputes between the states. Crucially, it could not raise any funds itself, and was entirely dependent on the states themselves for the money necessary to operate. Each state sent a delegation of between two and seven members to the Congress, and they voted as a bloc with each state getting one vote. But any decision of consequence required a unanimous vote, which led to a government that was paralyzed and ineffectual.
A movement to reform the Articles began, and invitations to attend a convention in Philadelphia to discuss changes to the Articles were sent to the state legislatures in 1787. In May of that year, delegates from 12 of the 13 states (Rhode Island sent no representatives) convened in Philadelphia to begin the work of redesigning government. The delegates to the Constitutional Convention quickly began work on drafting a new Constitution for the United States.
James Madison introduced 12 amendments to the First Congress in 1789. Ten of these would go on to become what we now consider to be the Bill of Rights. One was never passed, while another dealing with Congressional salaries was not ratified until 1992, when it became the 27th Amendment. Based on the Virginia Declaration of Rights, the English Bill of Rights, the writings of the Enlightenment, and the rights defined in the Magna Carta, the Bill of Rights contains rights that many today consider to be fundamental to America.
The U.S. Constitution guarantees many of the basic rights of citizens and legal residents, including free speech, religion, and due process. Due process is a lesser known, but extremely important, right. Under the due process clause, a U.S. citizen cannot lose their life, liberty, or property without notice and the opportunity to be heard. In a famous decision, Cruzan v. Director, Missouri Department of Health, the Supreme Court established that the due process clause protects a patient’s liberty to refuse medical treatment, even if that refusal would ultimately lead to the patient’s death.
Advance directives are legal documents that allow the patient to spell out their decisions about end-of-life care ahead of time. The rationale for these types of documents is that if there is nothing medically possible to prolong or improve the patients’ life, the patient would prefer to die than suffer the endless medical intervention or encumber his/her estate with debt (assuming there was one in the first place).
An Argument Only A Lawyer Could Love
So the patient has a right to choose what happens to their bodies even if they die. The argument that is made is that the patient can choose to give consent or refuse treatment based on the 4th Amendment to the Constitution which bans illegal search and seizure (by the government or anyone) and allows a person to be secure in their person, place, or property. The argument being the person’s body has a right to be secure in their own body. Probably not what was envisioned by the framers of the constitution who, enlightened by ideals of the Renaissance period and remembering all too well the tyrannical government of the British.
dnr-12O.C.G.A. § 31-39-3
§ 31-39-3. Patient presumed to consent to administration of cardiopulmonary resuscitation; patient's order not to resuscitate; health care facilities not required to expand to provide cardiopulmonary resuscitation (a) Every patient shall be presumed to consent to the administration of cardiopulmonary resuscitation in the event of cardiac or respiratory arrest, unless there is consent or authorization for the issuance of an order not to resuscitate. Such presumption of consent does not presume that every patient shall be administered cardiopulmonary resuscitation, but rather that every patient agrees to its administration unless it is medically futile. (b) Every adult shall be presumed to have the capacity to make a decision regarding cardiopulmonary resuscitation unless determined otherwise in writing in the patient's medical record pursuant to this Code section or pursuant to a court order. When an order not to resuscitate is requested by an adult with decision-making capacity, such order shall be presumed, unless revoked pursuant to Code Section 31-39-6, to be the direction of such person regarding resuscitation. (c) Nothing in this chapter shall require a health care facility, any other facility, or a health care provider to expand its existing equipment and facilities to provide cardiopulmonary resuscitation.
A ‘Do Not Resuscitation‘ (DNR) order is a written declaration by the patient who does not want some or all resuscitation measures in the event they deteriorate into cardiac arrest. The International Liaison Committee on Resuscitation (the international counterpart to the American Heart Heart Association, European Heart Association, etc.) recommends that the documentation of a DNR should be standardized, perhaps on a form provided by a government agency.
Patients also draft ‘Living Wills’ that more or less declare their wishes to not be resuscitated in the event of cardiac arrest or near cardiac arrest. What makes this type of document confusing is the fact it may not use standard language (probably written by an attorney) and would have to be interpreted by EMS personnel at the time of the call. Sometimes, advanced directives don’t really address EMS as much as it addresses the hospital. For whatever reason, the patient would be okay with EMS trying to resuscitate them, but not anyone at the hospital.
In lieu of having to make a decision, some patients relinquish the responsibility on a family member who makes the decision for them when the time comes. This type of document is called a durable power of attorney for healthcare or healthcare proxy. This ‘proxy’ would have the ability to make the decision for the patient when the time comes.
So what happens if the EMT doesn’t feel good about following the DNR or living will? In Georgia, any health care provider is protected from liability in the event they are attempting to resuscitate a patient with a valid DNR or living will. The only fact that must be proven by an attorney should a suit be pursued is that the health care provider provided the care in good faith.
O.C.G.A. § 31-39-7
§ 31-39-7. Liability of persons carrying out in good faith decisions regarding cardiopulmonary resuscitation; notification of next of kinor authorized person of patient by physician refusing to comply with order not to resuscitate (a) No physician, health care professional, nurse, physician assistant, caregiver, health care facility, other licensed facility, emergency medical technician, or person employed by, acting as the agent of, or under contract with any of the foregoing shall be subject to criminal prosecution or civil liability or be deemed to have engaged in unprofessional conduct for carrying out in good faith a decision regarding cardiopulmonary resuscitation authorized by this chapter by or on behalf of a patient or for those actions taken in compliance with the standards and procedures set forth in this chapter. (b) No physician, health care professional, nurse, physician assistant, caregiver, health care facility, other licensed facility, emergency medical technician, or person employed by, acting as the agent of, or under contract with any of the foregoing shall be subject to criminal prosecution or civil liability or be deemed to have engaged in unprofessional conduct for providing cardiopulmonary resuscitation to a patient for whom an order not to resuscitate has been issued, provided that such physician or person:(1) Reasonably and in good faith was unaware of the issuance of an order not to resuscitate; or (2) Reasonably and in good faith believed that consent to the order not to resuscitate had been revoked or canceled. (c) No persons shall be civilly liable for failing or refusing in good faith to effectuate an order not to resuscitate. No person shall be subject to criminal prosecution or civil liability for consenting or declining to consent in good faith, on behalf of a patient, to the issuance of an order not to resuscitate pursuant to this chapter. (d) Any attending physician who fails or refuses to comply with an order not to resuscitate entered pursuant to this chapter shall endeavor to advise promptly the patient, if conscious, or the next of kin or authorized person of the patient that such physician is unwilling to effectuate the order. The attending physician shall thereafter at the election of the next of kin or authorized person:(1) Make a good faith attempt to effect the transfer of the patient to another physician who will effectuate the order not to resuscitate; or (2) Permit the next of kin or authorized person to obtain another physician who will effectuate the order not to resuscitate. (e) Any emergency medical technician who fails or refuses to comply with an order not to resuscitate entered pursuant to this chapter shall endeavor to advise promptly the patient, if conscious, or the next of kin or authorized person of the patient, if reasonably available, that such emergency medical technician is unwilling to effectuate the order.
