Ectopic Pregnancy
Published .
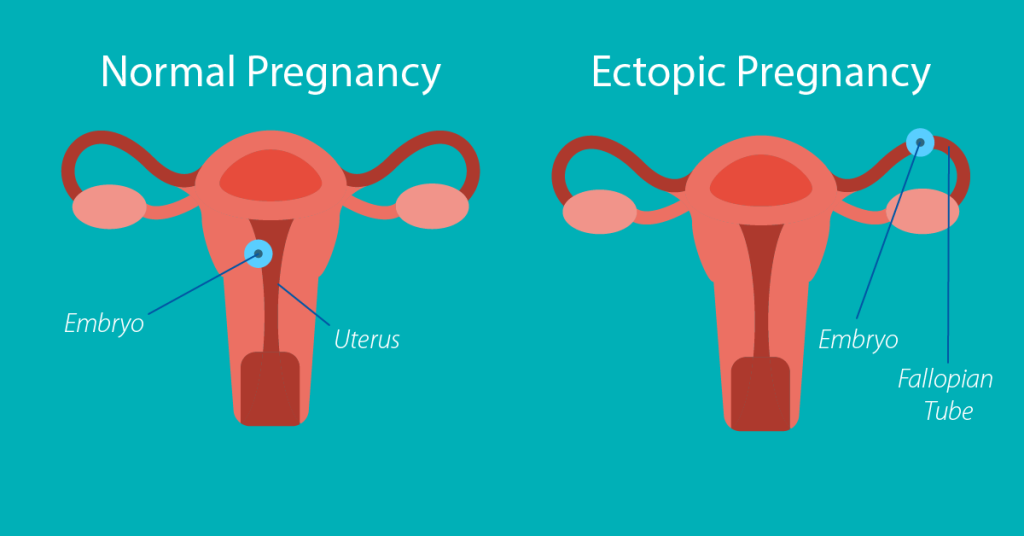
Ectopic pregnancy is a known complication of pregnancy that can carry a high rate of morbidity and mortality when not recognized and treated promptly. It is essential that providers maintain a high index of suspicion for an ectopic in their pregnant patients as they may present with pain, vaginal bleeding, or more vague complaints such as nausea and vomiting. Fertilization and embryo implantation involve an interplay of chemical, hormonal, and anatomical interactions and conditions to allow for a viable intrauterine pregnancy. Much of this system is outside the scope of this article but the most relevant anatomical components to our discussion on the ovaries, fallopian tubes, uterus, egg, and sperm. Ovaries are the female reproductive organs located to both lateral aspects of the uterus in the lower pelvic region. Ovaries serve multiple functions, one of which is to release an egg each month for potential fertilization. The fallopian tubes are tubular structures that serve as a conduit to allow transport of the female egg from the ovaries to the uterus. When sperm is introduced, it will fertilize the egg forming an embryo. The embryo will then implant into endometrial tissue within the uterus. An ectopic pregnancy occurs when this fetal tissue implants somewhere outside of the uterus or attaching to an abnormal or scarred portion of the uterus.
Etiology
Ectopic pregnancy, in essence, is the implantation of an embryo outside of the uterine cavity most commonly in the fallopian tube. Smooth muscle contraction and ciliary beat within the fallopian tubes to assist the transport of an oocyte and embryo. Damage to the fallopian tubes, usually secondary to inflammation, induces tubal dysfunction which can result in retention of an oocyte or embryo. There are several local factors, such as toxic, infectious, immunologic, and hormonal, that can induce inflammation.
Ectopic implantation can occur in the cervix, uterine cornea, myometrium, ovaries, abdominal cavity, etc. Women with tubal ligation or other post-surgical alterations to their fallopian tubes are at risk for ectopic pregnancies as the native function of the fallopian tube would be altered. The patient additionally can have an ectopic pregnancy with a concurrent intrauterine pregnancy, as known as a heterotopic pregnancy.
Epidemiology
The estimated rate of ectopic pregnancy in the general population is 1 to 2% and 2 to 5% among patients who utilized assisted reproductive technology. Ectopic pregnancies with implantation occurring outside of the fallopian tube account for less than 10% of all ectopic pregnancies. Cesarean scar ectopic pregnancies occur in 4% of all ectopic pregnancies, as well as 1 in 500 pregnancies in women who underwent at least one prior c-section. Interstitial ectopic pregnancies are reported in up to 4% of all ectopic implantation sites and have morbidity with mortality rates up to 7 times higher than other ectopic implantation sites. This increased morbidity and mortality are due to a high rate of hemorrhage in interstitial ectopic pregnancies. Intramural ectopic pregnancies, those implanted in the myometrium, were reported in 1% of ectopic pregnancies. Ectopic pregnancies implanting in the abdominal cavity account for 1.3% of ectopic implantation sites, of which adhere most commonly in the pouches anterior and posterior to the uterus as well as on the serosa of the adnexa and uterus. Reports also exist of implantation sites in omental, retroperitoneal, splenic, and hepatic locations.
Risk factors associated with ectopic pregnancies include advanced maternal age, smoking, history of ectopic pregnancy, tubal damage or tubal surgery, prior pelvic infections, DES exposure, IUD use, and assisted reproductive technologies. Older age does bear risk with ectopic pregnancy; aged fallopian tubes likely have relatively decreased function predisposing to delay of oocyte transport. Women with prior ectopic pregnancies have up to ten times risk compared to the general population. Women pursuing in vitro fertilization have increased risk with developing an ectopic pregnancy with a concurrent intrauterine pregnancy, as known as heterotypic pregnancy. The risk is estimated as high as 1:100 women pursuing in vitro fertilization. The risk of developing a heterotopic pregnancy has been estimated as high as 1:100 in women seeking in vitro fertilization.
Histopathology
The most common site for ectopic pregnancy adherence is in the ampullary region of the fallopian tube. Reportedly 95% of ectopic pregnancies develop in the ampulla, infundibular, and isthmic portions of the fallopian tubes. With cesarean scar pregnancies, there is a migration of blastocyst into the myometrium due to residual scarring defect from prior c-section. The depth of implantation determines the type of cesarean scar pregnancy with type 1 having proximity to the uterine wall and type 2 implanting closer to the urinary bladder.
History and Physical
Women presenting with an ectopic pregnancy will often complain of pelvic pain; however, not all ectopic pregnancies manifest with pain. Women of childbearing age who complain of pelvic pain/discomfort, abdominal pain/discomfort, nausea/vomiting, syncope, lightheadedness, vaginal bleeding, etc. should merit consideration for the possibility of pregnancy. Providers need to identify when the patient’s last menstrual period occurred and whether they have monthly routine menstrual periods. If patients have missed their last period or have abnormal uterine bleeding, and are sexually active, then they may be pregnant and thus need further testing with a pregnancy test. Providers should identify any known risk factors for ectopic pregnancy in their patient’s history, such as if a patient has had a prior confirmed ectopic pregnancy, known fallopian tube damage (history of pelvic inflammatory disease, tubal surgery, known obstruction), or achieved pregnancy through infertility treatment.
After obtaining a thorough history, an attentive physical exam is the next step. Evaluation of vital signs to assess for tachycardia and hypotension is pivotal in determining the patient’s hemodynamic stability. When examining the abdomen and suprapubic regions, attention should focus on the location of tenderness as well as any exacerbating factors. If voluntary/involuntary guarding of the abdominal musculature is elicited on palpation, this should raise concern for possible free fluid or other cause of peritoneal signs. Palpating a gravid uterus may suggest pregnancy, however, does not exclude other pathologies such as progressed ectopic pregnancy or heterotopic pregnancy. Patient’s presenting with vaginal bleeding would likely benefit from a pelvic exam to assess for infections as well as assess the cervical os. Bimanual pelvic exams additionally allow for palpation of bilateral adnexa to assess for any abnormal masses/structures or to elicit adnexal tenderness. A thorough history and physical exam will lend better certainty with testing obtained when evaluating for possible ectopic pregnancy.
