Upper GI Bleed
Published .
ligament of Treitz
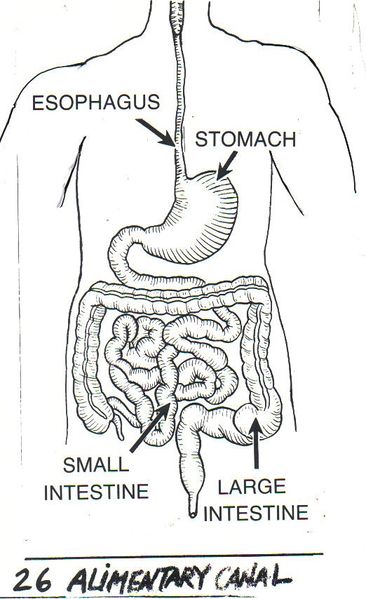
Upper gastrointestinal bleeding (UGIB) is a common problem with an annual incidence of approximately 80 to 150 per 100,000 population, with estimated mortality rates between 2% to 15%. UGIB is classified as any blood loss from a gastrointestinal source above the ligament of Treitz. It can manifest as hematemesis (bright red emesis or coffee-ground emesis), hematochezia, or melena. Patients can also present with symptoms secondary to blood loss, such as syncopal episodes, fatigue, and weakness. UGIB can be acute, occult, or obscure.
Etiology
From the possible etiologies of UGIB, Peptic Ulcer disease (PUD) accounts for 40% to 50% of the cases. Of those, the majority is secondary to duodenal ulcers (30%). PUD can be associated with NSAIDs, Helicobacter pylori, and stress-related mucosal disease.
Aside from PUD, erosive esophagitis accounts for 11%, duodenitis for 10%, Varices 5% to 30% (depending if the population studied have a chronic liver disease), Mallory-Weiss tear 5% to 15% and vascular malformations for 5%.
Epidemiology
UGIB accounts for 75% of all acute gastrointestinal (GI) bleeding cases. Its annual incidence is approximately 80 to 150 per 100,000 population. Patients on long-term, low-dose aspirin have a higher risk of overt UGIB compared to placebo. When aspirin is combined with P2Y12 inhibitors such as clopidogrel, there is a two-fold to three-fold increase in the number of UGIB cases. When a patient requires triple therapy (i.e., aspirin, P2Y12 inhibitor and vitamin K antagonist), the risk of UGIB is even higher.
History and Physical
During history taking, attention should be given to comorbidities. A detailed review of current medications should be performed, and patients should be directly asked about the use of NSAIDs, antiplatelet drugs, aspirin, or anticoagulants. Also, it is important to get a detailed social history regarding alcohol use.
The clinical presentation can vary but should be well-characterized. Hematemesis is the overt bleeding with vomiting of fresh blood or clots. Melena refers to dark and tarry-appearing stools with a distinctive smell. The term “coffee-grounds” describes gastric aspirate or vomitus that contains dark specks of old blood. Hematochezia is the passage of fresh blood per rectum. The latter is usually a reflection of lower gastrointestinal bleeding (LGIB) but may be seen in patients with brisk UGIB.
Patients may also present with syncope or orthostatic hypotension if bleeding is severe enough to cause hemodynamic instability.
One should also pay attention to the patient’s vital signs. Orthostatic vital signs should also be documented. In a comprehensive exam, search for evidence of chronic liver diseases such as palmar erythema, spider angiomas, gynecomastia, jaundice, and ascites. These features may give clues to the etiology of the bleeding (i.e., variceal bleeding).
