Lower GI Bleed
Published .
Gastrointestinal (GI) bleeding is a term used for any bleeding that occurs within the GI tract from mouth to anus. GI bleeding can be categorized into upper and lower in origin. The ligament of Treitz is commonly used as the point to differentiate the two. Bleeds proximal to the ligament are upper GI bleeds, and distal bleeds are lower GI bleeds. Categorization into one of the two groups is important as it directs the evaluation and management of the patient.
Etiology
Lower GI bleeds can be categorized further into three types: massive, moderate, and occult bleeding.
Massive bleeding usually occurs in patients older than 65 years with multiple medical problems, and this bleeding presents as hematochezia or bright red blood per rectum. The patient is usually hemodynamically unstable with a systolic blood pressure (SBP) equal to or less than 90 mmHg, heart rate (HR) less than or equal 100/min, and low urine output. Massive lower GI bleeds are mostly due to diverticulosis and angiodysplasias. The mortality rate may be as high as 21%.
Moderate bleeding can occur at any age and presents as hematochezia or melena. The patient is usually hemodynamically stable. Many disease processes should be considered on the differential list including neoplastic disease, inflammatory, infectious, benign anorectal, and congenital.
Finally, occult lower GI bleeds can present in patients at any age. Lab work reveals patients with microcytic hypochromic anemia due to chronic blood loss. The differential diagnosis of these patients should include inflammatory, neoplastic and congenital. The patient typically appears well, hemodynamically stable.
Epidemiology
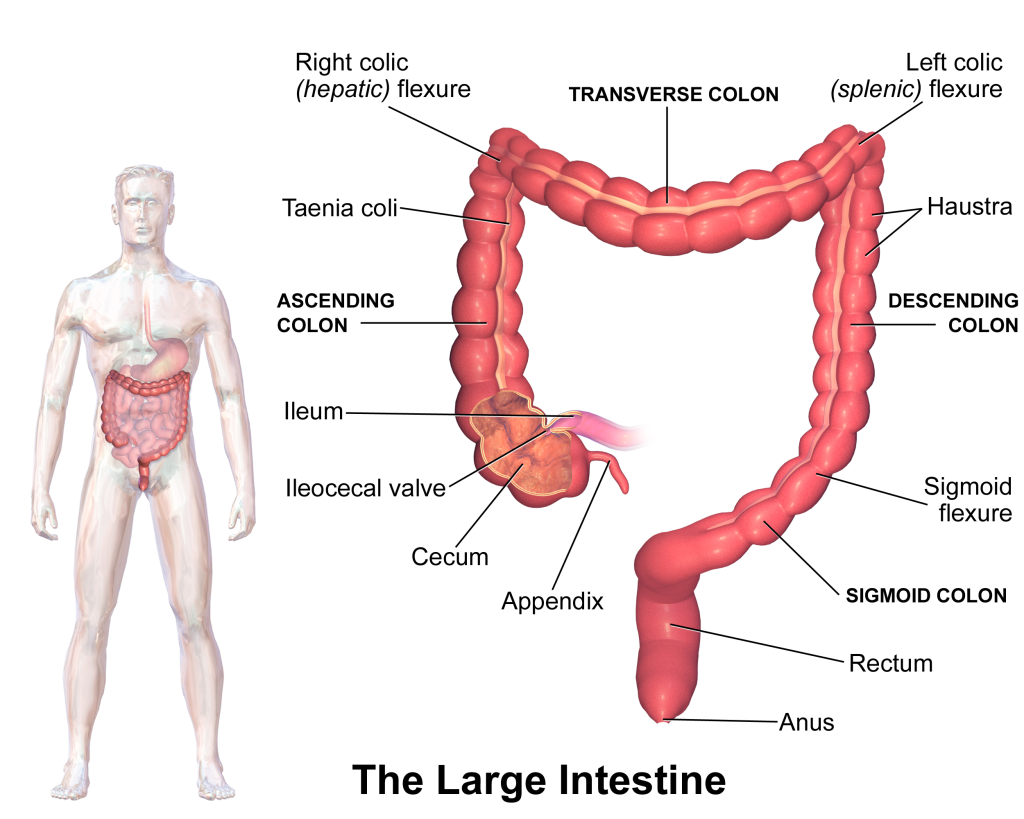
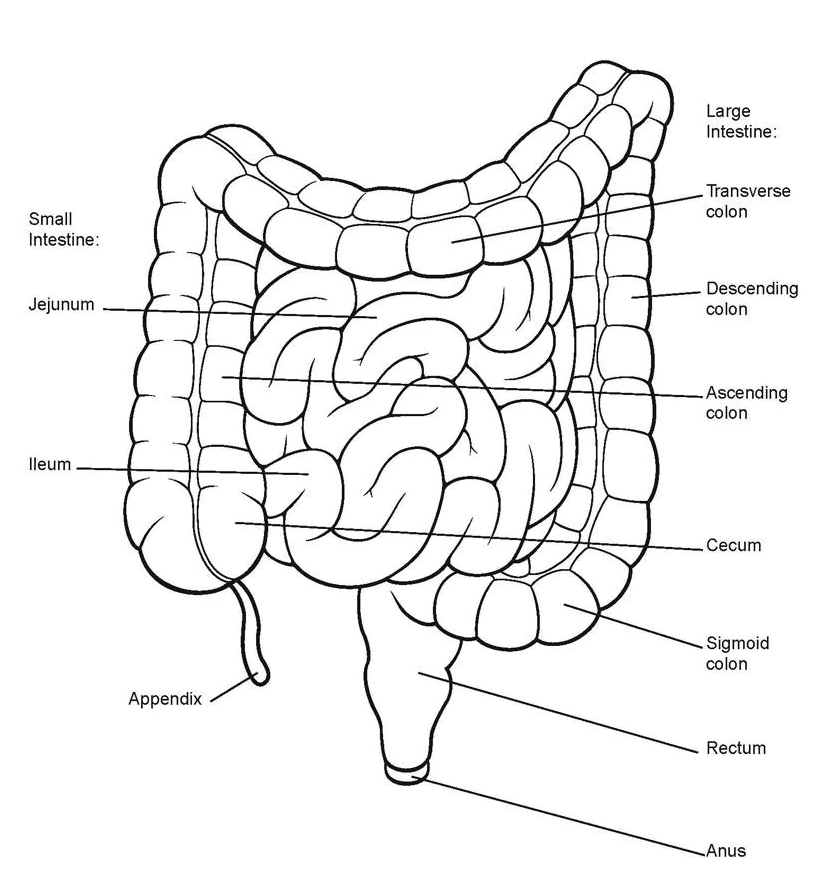
Lower GI bleeds are fairly common and account for 20% to 30% of all patients presenting with major GI bleeding. The incidence is higher in older patients and patients taking multiple medications or multi-pharmacy. Approximately, 80% to 85% of lower GI bleeds originate distal to the ileocaecal valve, with only 0.7% to 9% originating from the small intestine. The remaining cases usually begin in the upper GI tract. These patients usually present with brisk bleeding, melena, or bright red blood per rectum.
Pathophysiology
The diverticular disease accounts for over 40% of lower GI bleeds and often presents as painless hematochezia. More than 80% of lower GI bleeds will stop spontaneously, and overall mortality has been noted to be 2% to 4%. Diverticular bleeding usually recurs. Therefore early identification and management are imperative. The prevalence of diverticular disease increases in elderly patients, particularly ages older than 80 years, patients with chronic constipation, and altered colonic motility. The left colon is often more commonly affected as being the source of diverticular bleeds.
Approximately, one-third of patients with presumed lower GI bleeds and heavy bleeding will have an upper GI bleed, particularly, if the patient presents with signs and symptoms of peptic ulcer disease or recent (non-steroidal anti-inflammatory) NSAID use. Ischemic colitis occurs in 20% of lower GI bleeds and is more prevalent in the elderly. It occurs in response to reduced mesenteric flow to the colon due to decreased cardiac output, vasospasm, or atherosclerotic disease. Non-thrombotic causes usually affect the watershed areas of the bowel, notably, the splenic flexure. These non-occlusive disease processes usually resolve with hydration and nonsurgical intervention. Occlusive or thromboembolic events can affect much larger areas of the bowel and should be quickly evaluated with mesenteric angiography. Patients with mesenteric ischemia require radiographic and/or surgical evaluation and intervention.
The most common cause of lower GI bleeds in patients younger than 50 years is anorectal disorders, specifically, hemorrhoids. Inflammatory bowel disease (IBD) and NSAID use should also be evaluated in lower GI bleeds. Other disease processes practitioners should consider include vascular ectasias which are flat, red mucosal lesions in the cecum and ascending colon and represent 10% of lower GI bleeds. Post-polypectomy bleeding is more common in patients older than 65 years with a polyp greater than 1 cm. Bleeding is usually self-limited but can be delayed up to one week after the procedure.
History and Physical
Patients presenting with lower GI bleeds can have varying symptoms and signs. Therefore a thorough history is necessary. Patients can present with scant bleeding to massive hemorrhage. Key details in the history should include whether the bleeding is recurrent or sporadic if there are associated symptoms and a detailed review of the patient’s medications including, antiplatelets, anticoagulants, and NSAIDs. The family history of colon cancer or inflammatory bowel disease (IBD) should also be noted.
Abdominal examination and digital rectal examination should be completed in all patients presenting with lower GI bleeds. If available, consider proctoscopy as well. Abdominal examination may reveal tenderness, distension, or a mass depending on the cause. When completing the digital rectal examination (DRE) inspect for hematochezia and anorectal pathology, such as hemorrhoids. Studies reveal that left colonic bleeding tends to be bright red, whereas right colonic is usually maroon and may be accompanied with clots. However noted in practice, bright red blood per rectum can occur in right-sided bleeds that are brisk and massive.
Treatment / Management
Colonoscopy has been shown to correctly identify the source of lower GI bleeds in more than 75% of patients while also allowing a therapeutic modality. The timing of the colonoscopy remains controversial. However, most studies suggest it should be performed within the first 24 hours of admission, following bowel prep of the patient. Treatments for diverticular bleeds include the injection of adrenaline (1:10000) in 1 mL to 2mL aliquots at the site. If the patient is not stable enough for a colonoscopy, then radiologic evaluation should be considered. CT angiography (CTA) is relatively noninvasive, fast and widely available. CTA can detect bleeding rates more than .3 mL/min to .5 mL/min. CTA, however, has a relatively low sensitivity (85%). Catheter angiography is reserved for patients with hemodynamic instability who cannot tolerate a colonoscopy or have recurrent bleeding. Radionuclide imaging uses Technetium (99mTc) based tracers to tag red blood cells and is helpful in detecting scant intermittent bleeding. The half-life of 99mTc is long so the scan can be repeated several times in a 24-hour period to evaluate sequential images. Surgery may be required if radiologic and endoscopic procedures fail. It is best to consult a colorectal surgeon early in the diagnostic evaluation of the patient as these patients and become unstable fairly quickly. In patients with hemodynamic instability, requiring more than six units of blood within 24 hours, or not responding to resuscitation attempts, emergency segmental resection or subtotal colectomy may be required.
