Epidural Hematoma
Published (updated: ).
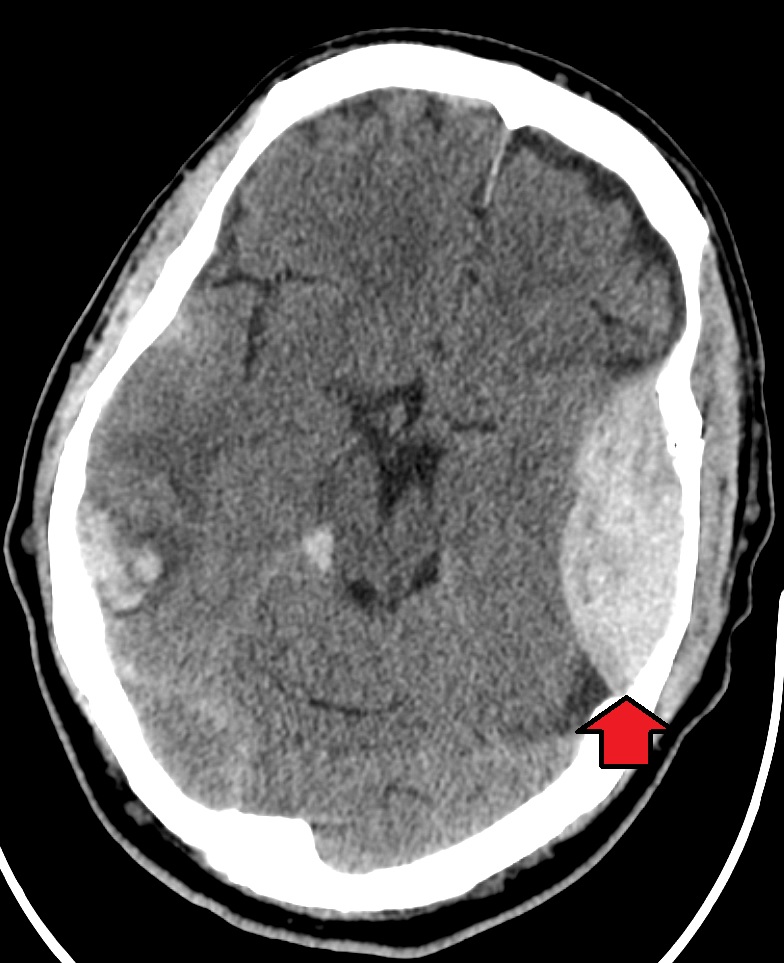
An epidural hematoma (EDH) is an extra-axial collection of blood within the potential space between the outer layer of the dura mater and the inner table of the skull. It is confined by the lateral sutures (especially the coronal sutures) where the dura inserts. It is a life-threatening condition, which may require immediate intervention and can be associated with significant morbidity and mortality if left untreated. Rapid diagnosis and evacuation are important for a good outcome.
Etiology
It occurs in approximately 10% of traumatic brain injuries (TBI) requiring hospitalization. Both traumatic and non-traumatic mechanisms can cause an epidural hematoma.
The majority of cases related to a traumatic mechanism are a result of head injury due to motor vehicle collisions, physical assaults, or accidental falls.
Non-traumatic mechanisms include the following:
- Infection/Abscess
- Coagulopathy
- Hemorrhagic Tumors
- Vascular Malformations
Epidemiology
An epidural hematoma occurs in 2% of all head injuries and up to 15% of all fatal head traumas. Males are more often affected than are females. Furthermore, the incidence is higher among adolescents and young adults. The mean age of affected patients is 20 to 30 years, and it is rare after 50 to 60 years of age. As an individual’s age advances, the dura mater becomes more adherent to the overlying bone. This decreases the chance that a hematoma can develop in the space between the cranium and dura.
Pathophysiology
Arterial Injury
Most epidural hematomas result from arterial bleeding from a branch of the middle meningeal artery. The anterior meningeal artery or dural arteriovenous (AV) fistula at the vertex may be involved.
Venous Injury
Up to 10% of EDHs are due to venous bleeding following the laceration of a dural venous sinus.
In adults, up to 75% of EDHs occur in the temporal region. However, in children, they occur with similar frequency in the temporal, occipital, frontal, and posterior fossa regions.
A skull fracture is present in the majority of patients with EDH. These hematomas often present beneath a fracture of the squamous part of the temporal bone.
If this condition occurs within the spine, this entity is described as a spinal epidural hematoma.
Based on radiographic progression, it can be classified into one of the following
- Type I: Acute; occurs on day 1 and associated with a “swirl” of un-clotted blood
- Type II: Subacute occurring between days 2 to 4 and usually solid
- Type III: Chronic occurring between days 7 to 20; mixed or lucent appearance with contrast enhancement
History and Physical
The typical presentation is an initial loss of consciousness following trauma, a complete transient recovery (“often termed as a lucid interval”), culminating in a rapid progression of neurological deterioration. This occurs in 14% to 21% of patients with an EDH. However, these patients may be unconscious from the beginning or may regain consciousness after a brief coma or may have no loss of consciousness. Therefore, the presentations range from a temporary loss of consciousness to a coma. Beware that the lucid interval is not pathognomonic for an EDH and may occur in patients who sustain other expanding mass lesions. The classic lucid interval occurs in pure EDHs that are very large and demonstrate a CT scan finding of active bleeding. The presentation of symptoms depends on how quickly the EDH is developing within the cranial vault. A patient with a small EDH may be asymptomatic, but this is rare. Also, an EDH may also develop in a delayed fashion.
This enlarging hematoma leads to eventual elevation of intracranial pressure which may be detected in a clinical setting by observing ipsilateral pupil dilation (secondary to uncal herniation and oculomotor nerve compression), the presence of elevated blood pressure, slowed heart rate, and irregular breathing. This triad is known as the “Cushing reflex.” These findings may indicate the need for immediate intracranial intervention to prevent central nervous system (CNS) depression and death.
Treatment / Management
EDH is a neurosurgical emergency. It, therefore, requires urgent surgical evacuation to prevent irreversible neurological injury and death secondary to hematoma expansion and herniation. Neurosurgical consultation should be urgently obtained as it is important to intervene within 1 to 2 hours of presentation.
Differential Diagnosis
- Intracranial abscess
- Intracranial mass
- Seizure
- Transient ischemic attack
Complications
- Mass effect: compression of the brain if bleeding is significant
- Herniation
- Seizures
