Diffuse Axonal Injury
Published .
Diffuse axonal injury (DAI) is a type of traumatic brain injury (TBI) that results from a blunt injury to the brain. In the United States, traumatic brain injury is a leading cause of death and disability among children and young adults. The Center for Disease Control and Prevention (CDC) estimates that there are over 1.5 million reported cases of traumatic brain injury every year in the United States. Traumatic brain injury is classified as mild, moderate, and severe based on the Glasgow coma scale (GCS). Traumatic brain injury patients with GCS of 13 to 15 are classified to be mild, which includes the majority of traumatic brain injury patients. Patients with a GCS of nine to 12 are considered to have a moderate traumatic brain injury, while patients with a GCS below eight are classified as having a severe traumatic brain injury.
The GCS measures the following three functions:
- Eye Opening (E): 4-spontaneous, 3-to voice, 2-to pain, 1-none
- Verbal Response (V): 5-normal conversation, 4-oriented conversation, 3-words, but not coherent, 2-no words, only sounds, 1-none
- Motor Response (M): 6-normal, 5-localized to pain, 4-withdraws to pain, 3-decorticate posture, 2-decerebrate
Diffuse axonal injury (DAI) primarily affects the white matter tracts in the brain. Clinically, patients with DAI can present in a spectrum of neurological dysfunction. This can range from clinically insignificant to a comatose state. However, most patients with DAI are identified to be severe and commonly have a GCS of less than 8. A diffuse axonal injury is a clinical diagnosis.
Etiology
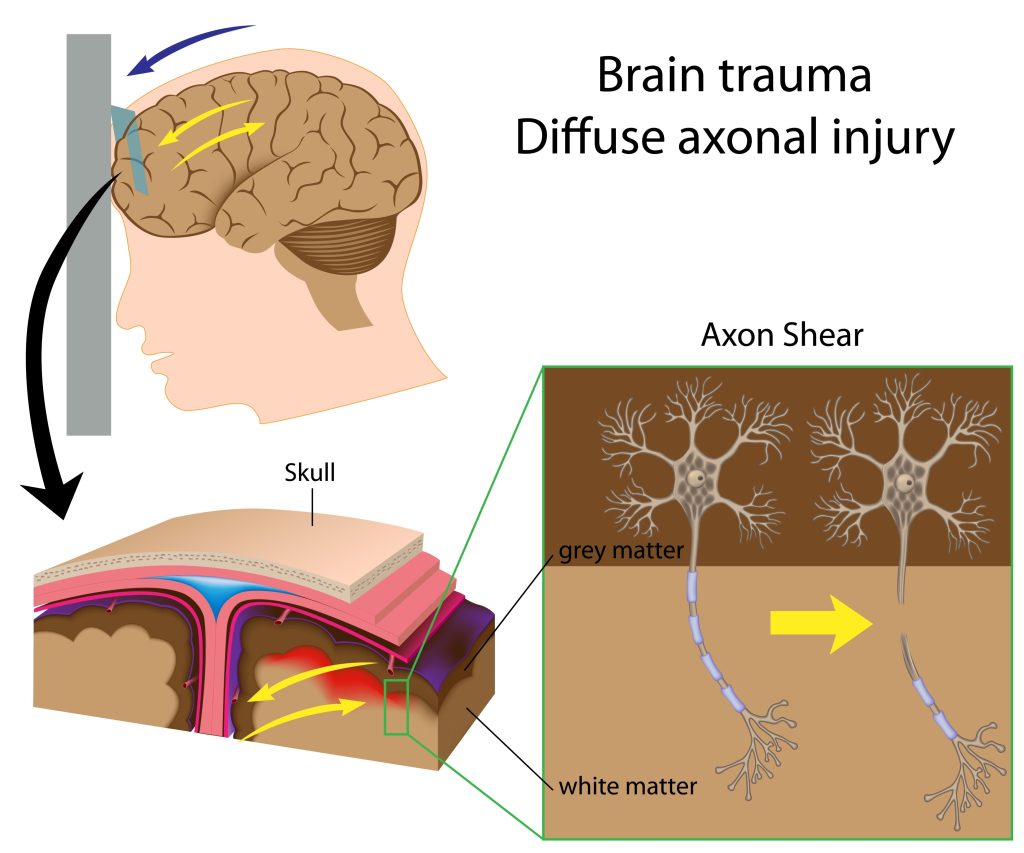
The most common etiology of diffuse axonal injury involves high-speed motor vehicle accidents. The most common mechanism involves an accelerating and decelerating motion that leads to shearing forces to the white matter tracts of the brain. This leads to microscopic and gross damage to the axons in the brain at the junction of the gray and white matter. Diffuse axonal injury commonly affects white matter tracts involved in the corpus callosum and brainstem. Interestingly, there is no association between diffuse axonal injury and underlying skull fractures.
Epidemiology
The true incidence of DAI is unknown. However, it is estimated that roughly 10% of all patients with TBI admitted to the hospital will have some degree of DAI. Of the patients with DIA, it is estimated that roughly 25% will result in death. This statistic may be underestimated as patients with subdural hematomas, epidural hematomas, and other forms of TBI will not carry a true diagnosis of DAI. Postmortem studies have shown that patients with severe TBI have a significant incidence of diffuse axonal injury.
Pathophysiology
The primary insults of diffuse axonal injury lead to disconnection or malfunction of neuron’s interconnection. This affects numerous functional areas of the brain. Usually, patients with diffuse axonal injury present with bilateral neurological examination deficits frequently affecting the frontal and temporal white matter, corpus callosum, and brainstem. The Adams classification of diffuse axonal injury utilizes pathophysiological lesions in the white matter tracts and clinical presentation.
The Adams Diffuse Axonal Injury Classification
- Grade 1: A mild diffuse axonal injury with microscopic white matter changes in the cerebral cortex, corpus callosum, and brainstem
- Grade 2: A moderate diffuse axonal injury with gross focal lesions in the corpus callosum
- Grade 3: A severe diffuse axonal injury with finding as Grade 2 and additional focal lesions in the brainstem
Histopathology
Axonal portions of neurons have a mechanical disruption of cytoskeletons resulting in proteolysis, swelling, and other microscopic and molecular changes to the neuronal structure.
History and Physical
DAI is a clinical diagnosis. Typically, DAI is considered in patients with a GCS of less than 8 for over six hours. The clinical presentation of patients with diffuse axonal injury relates to the severity of a diffuse axonal injury. For example, patients with mild diffuse axonal injury present with signs and symptoms that reflect a concussive disorder. These symptoms most commonly include a headache. The other post-concussive symptoms can include dizziness, nausea, vomiting, and fatigue. However, patients with a severe diffuse axonal injury may also present with a loss of consciousness and remain in a persistent vegetative state. A very small number of those patients with severe diffuse axonal injury will regain consciousness in the first year after the injury.
Other common neurological manifestations include dysautonomia. Dysautonomic symptoms commonly include tachycardia, tachypnea, diaphoresis, vasoplegia, hyperthermia, abnormal muscle tone, and posturing.
Evaluation
In general, diffuse axonal injury is a severe form of traumatic brain injury. Therefore, the implementation of an advanced trauma life support protocol is a standard of care for all head-injured patients.
A definitive diagnosis of diffuse axonal injury can be made in the postmortem pathologic examination of brain tissue. However, in clinical practice, a diagnosis of diffuse axonal injury is made by implementing clinical information and radiographic findings. Understanding the mechanism of head injury facilitates a differential diagnosis of DAI. Patients who experience rotational or acceleration-deceleration closed head injury should be suspected to have DAI. Generally, DAI is diagnosed after a traumatic brain injury with GCS less than 8 for more than six consecutive hours.
Radiographically, computed tomography (CT) head findings of small punctate hemorrhages to white matter tracts can indicate diffuse axonal injury in the setting of an appropriate clinical presentation. Overall, CT head has a low yield in detecting diffuse axonal injury-related injuries. Currently, magnetic resonance imaging (MRI), specifically diffuse tensor imaging (DTI), is the imaging modality of choice for the diagnosis of diffuse axonal injury. A recent report suggests that acute gradient-recalled echo (GRD) MRI will enhance the detection of axonal injury in grade 3 diffuse axonal injury patients, suggesting that it is most likely a better diagnostic tool.
It should be of note that DAI should be strongly considered in patients that fail to improve after receiving surgical evacuation of subdural or epidural hematomas. Conversely, if patients drastically improve after surgical evacuation of a subdural or epidural hematoma, DAI may not be present.
Currently, there are no laboratory tests for the diagnosis of DAI. However, there is current research on identifying molecular markers in the serum of traumatic brain injury patients to help aid the diagnosis of DAI.
Treatment / Management
Treatment of patients with diffuse axonal injury is geared toward the prevention of secondary injuries and facilitating rehabilitation. It appears to be the secondary injuries that lead to increased mortality. These can include hypoxia with coexistent hypotension, edema, and intracranial hypertension. Therefore, prompt care to avoid hypotension, hypoxia, cerebral edema, and elevated intracranial pressure (ICP) is advised.
Initial treatment priority in traumatic brain injury is focused on resuscitation. In a non-neuro trauma center, trauma surgeons and emergency physicians may perform the initial resuscitation and neurologic treatment to stabilize and transport the patient to a designated neurotrauma center expeditiously. ICP monitoring is indicated in patients with a GCS of less than 8 after consultation with neurosurgery. Other considerations for ICP monitoring include patients that cannot have continual neurologic evaluations. These are typically in patients receiving general anesthesia, opioid analgesia, sedation, and prolonged paralysis for other injuries. Cerebral oxygen saturation monitoring can be used with ICP monitoring to assess the degree of oxygenation. Short-term, usually seven days, anticonvulsant treatment can be used to prevent early post-traumatic seizures. There is no evidence that this will prevent long-term post-traumatic seizures, however. There is emerging evidence that progesterone treatment in acute traumatic brain injury may reduce morbidity and mortality. This cannot be routinely recommended at this time.
Overall, the goal of the treatment of patients with diffuse axonal injury is supportive care and prevention of secondary injuries.
Differential Diagnosis
- Subdural hematoma
- Epidural hematoma
- Subarachnoid hemorrhage
- Various Intracerebral hemorrhage types
- Ischemic and hemorrhagic cerebrovascular accident
- Concussion/post-concussive syndrome
- Hypoglycemia
Prognosis
Prognosis is considered to be poor in patients with severe DAI.
Complications
Dysautonomia is frequently encountered. Unfortunately, no definitive treatment exists, and supportive care is advised.
