Traumatic Brain Injury
Published .
Traumatic Brain Injury (TBI) may result from anywhere between a simple blow to the head to a penetrating injury to the brain. In the United States, around 1.7 million people suffer TBI with older adolescents (ages 15 to 19 years) and older adults (ages 65 years and older) among the most likely to sustain a TBI. The frontal and temporal areas of the brain are the main areas involved. Mild TBI (mTBI), also known as brain concussion, initially considered as a benign event, has galvanized tremendous attention for some of its adverse neuropsychological outcomes in civilians (e.g., athletes who play contact sports) as well as military personnel. Moderate to severe TBI is a primary cause of injury-induced death and disability. In the United States, It has an annual incidence of approximately 500 in 100,000. However, around 80% of all TBI cases are categorized as mild head injuries.
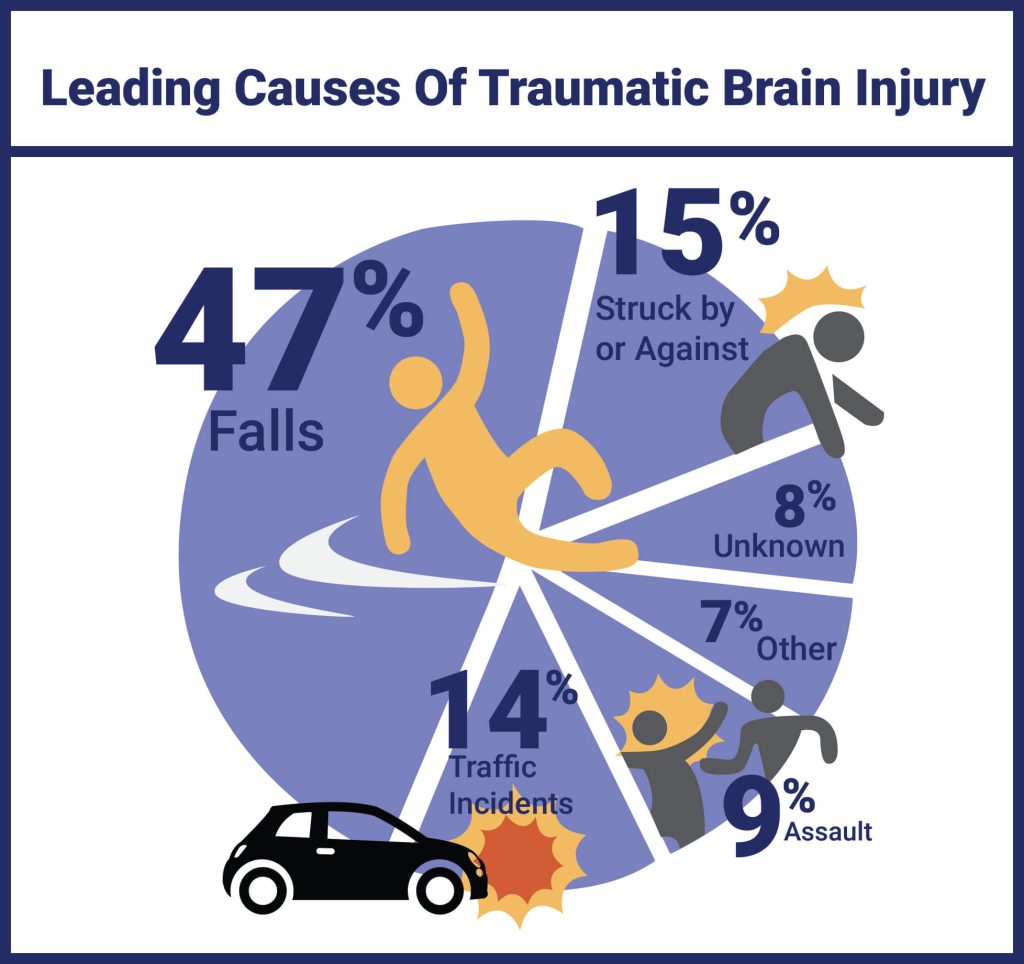
Etiology
Mild TBI or brain concussion usually results from closed brain injuries, the incident when the head is being struck by an object, such as a bat or a fist during a fight or when the head is affected by a nearby blast or explosion. Such injuries have shown to affect the structural integrity of the neurons.
Epidemiology
The male to female ratio is 2:1. A private study of 1084 individuals with traumatic brain injuries revealed that TBI was a high-risk factor not only for post-traumatic stress disorder (PTSD) but also for other psychiatric disorders. Statistically, the Center for Disease Control and Prevention (CDC) has estimated that annually, about 1.5 million Americans survive a traumatic brain injury (TBI). Among these, approximately 230,000 are hospitalized. In 2000, there were 10,958 TBI diagnoses. In 2015, this number jumped to 344,030. Mortality across all TBI severities is approximately 3%, yet morbidity is more difficult to estimate.
Pathophysiology
The Monro-Kellie hypothesis states that the total intracranial volume (composed of brain tissue, cerebrospinal fluid, venous blood, and arterial blood) should always remain a constant since the cranium is a rigid and non-expansile container. When an additional compartment is introduced (like a hematoma), there must be a compensatory reduction in another compartment in order to prevent intracranial hypertension. Cerebral perfusion pressure (CPP) is defined as mean arterial pressure (MAP) – intracranial pressure (ICP). When the ICP increases, the CPP will be reduced and can lead to secondary cerebral ischemia and infarct. The goal of TBI management is to prevent this secondary insult. The following are the different types of TBI commonly encountered:
Concussion
This is usually a mild TBI without any gross structural damage and occurs secondary to a nonpenetrating TBI. It usually results from acceleration/deceleration forces occurring secondary to a direct blow to the head. It causes a transient altered mental status, which can range from confusion to loss of consciousness. This cannot be diagnosed with a routine computed tomogram (CT) scan or magnetic resonance imaging (MRI) scan. Special sequence MRI like diffusion tensor imaging and functional MRI may result in earlier diagnosis of concussion.
Second impact syndrome: The initial event is often a concussion, but if the patient (often an athlete) starts to play without fully recovering from this and sustains another injury, there can be a rapid evolution of malignant cerebral edema, ensuing over a short-time course of time.
Chronic Traumatic Encephalopathy (CTE): This is usually a delayed manifestation of repetitive mild TBI. This is common in athletes and can lead to psychiatric disturbances and suicidal behavior, attention deficits, and derangements in memory and executive functions.
Extra-axial Hematoma
Extra-axial hematomas include both epidural hematomas (EDH) and subdural hematomas (SDH). EDH usually results from bleeding from the middle meningeal artery and its branches or a fracture and is usually acute. SDH can result from the bleeding of a bridging vein and can be acute or chronic.
Contusion
Contusions (bruising of the brain) can be a coup or contrecoup type. Coup contusions occur at the site of impact, whereas contrecoup injuries typically take place on the contralateral side of impact, usually the basi-frontal lobe and anterior temporal lobe.
Traumatic Subarachnoid Hemorrhage (SAH)
Subarachnoid hemorrhage is most commonly caused by trauma and results from the tearing of small capillaries with blood subsequently entering into the subarachnoid space. It commonly occurs over the convexity, whereas SAH secondary to aneurysmal rupture occurs in the basal cisterns.
Diffuse Axonal Injury (DAI)
This can underlie mild to moderate TBI and potentially results from any shearing, stretching, or twisting injuries to the neuronal axons. This phenomenon is mainly seen at the junction of the gray and white matter where neuronal axons are entering a more dense, fatty (myelinated), and less fluid-filled white matter. Such shearing forces cause the neuronal axon to be stretched, and the subsequent damage to the cytoskeleton may lead to axonal swelling, increased permeability, calcium influx, detachment, and axonal death. Diffuse laminar necrosis is typically seen on autopsy.
Treatments
Hyperbaric Oxygen Therapy (HBO2)
Some researchers discussed the role of oxygen delivered at supraphysiological amounts in the treatment of TBI. A study published in 2010 included closed-head trauma victims with GCS scores of 3 to 8 after resuscitation, without effects from paralytics, sedation, alcohol, and/or street drugs. HBO2 treatment began within 24 hrs post-injury admission to hospital with a mild or moderate TBI compared the effect of HBO2 to normobaric oxygen. They found a significant post-treatment effect of HBO2 on cerebral oxidative metabolism due to its ability to produce a brain tissue PO2 greater than or equal to 200 mmHg (higher cerebral blood flow lead to higher PO2, lower levels of lactate by 13% compared to control group, and lower intracranial pressure). However, in severe TBI, it is not an all or nothing phenomenon but represents a graduated effect. Some controversy still surrounds the use of HBO2 due to the limitations of studies such as the lack of blinding to the intervention, cost, time-consuming practice, and the validity of the actual diagnoses of the patients with reported TBI and PTSD who had a subsequent improvement.
Hypothermia

Studies have shown some controversy in the practicality of this practice depending on the patient’s characteristics (age, the initial GCS, the presence or absence of pupillary abnormalities, and CT-based classification of the severity of the injury). In general, there has been an increased belief that cooling the body to systemic temperatures around 34 C to 35 C, helps reduce secondary injury and improve behavioral outcomes. Studies have suggested that this occurs because of the ability of hypothermia to suppress the post-traumatic inflammatory response, in turn, preserving the blood-brain barrier and reducing the number of cytokines released as well as glutamate.
Medical Measures to Reduce Intracranial Pressure
Head end of bed elevation to 30 degrees, transient hyperventilation, hyperosmolar therapy, therapeutic cooling, and medically induced comatose state are some measures to reduce intracranial pressure. Some patients will need monitoring of the intracranial pressure..
Surgical Measures to Reduce Intracranial Pressure
This involves the evacuation of intracranial hematoma or decompressive craniectomy.
Differential Diagnosis
- Stroke
- Spontaneous acute subdural hematoma
- Alzheimer disease
- Anterior circulation stroke
- Brain metastasis
- Cerebral aneurysms
- Frontal lobe syndrome
- Hydrocephalus
Prognosis
Each year in the US, nearly 52,000 deaths occur as a result of TBI. Individuals who arrive with low GCS have the worst outcomes. Even those who survive have prolonged recovery and some are still left with residual neurological deficits. Complete recovery can take months or even years.
Complications
- Post-traumatic seizures
- Deep vein thrombosis
- Hydrocephalus
- Spasticity
- Mood and behavior changes
- Gait abnormalities
- Cognitive decline
- PTSD
- Post-traumatic headache
- Insomnia
