Battle’s Sign
Published (updated: ).

Battle Sign (also called Battle’s Sign) is defined as bruising over the mastoid process. It is retroauricular or mastoid ecchymosis that is typically the result of head trauma.
Battle sign derives its name from Dr. William Henry Battle who initially described the sign in the late 1800s. He was an English surgeon who initially described the ecchymosis in 17 patients who had head injuries with fractures to the posterior aspect of the skull base. His description noted that to develop the sign, there was significant head trauma and may indicate significant internal injury to the brain and not just the posterior cranial vault or mastoid.
Etiology
One of the most important issues associated with Battle sign is that it takes 1 to -2 days for the sign to appear and is thus not helpful in the initial management of head trauma.
The naming of the Battle sign has caused much confusion over the years. Many believe that the sign gets its name from fighting or battling as a mechanism for obtaining the injury instead of the credit going to Dr. Battle. Additionally, although Dr. Battle is credited with the sign and has his name on the sign, he was not the first to note the sign. Sir Prescott G. Hewett, an English surgeon, had actually written about the association before Dr. Battle.
Battle sign may be confused with a spreading hematoma from a fracture of the mandibular condyle, which is a less serious injury.
Another issue surrounding Battle sign is that there was a recent case report that showed mastoid ecchymosis associated with hepatic encephalopathy in the absence of trauma. This case means that Battle sign may not be as specific for head trauma as initially thought. However, more research is necessary regarding the association between hepatic encephalopathy and mastoid ecchymosis.
Epidemiology
Basilar skull fractures are present in only 4% of patients with a severe head injury. There is no reported increased predilection amongst either sex or any race. Battle sign typically correlates with blunt head trauma; this is most commonly accidental but may also be present in non-accidental head trauma, including in child abuse.
Overall the majority of skull-based fractures are linear and tend to be more common in children. The temporal bone is involved in the majority of skull fractures (45%), followed by basilar skull fractures (20%). When a depressed skull fracture occurs, it is usually an open fracture, which generally necessitates surgery as soon as possible.
Pathophysiology
Battle sign is prominent when there is a fracture of the petrous temporal bone. It may also be associated with rhinorrhea and bruising over the eyes (raccoon eyes). Depending on the severity of the head trauma, the patient may also present with loss of consciousness and a depressed Glasgow coma scale (GCS).
History and Physical
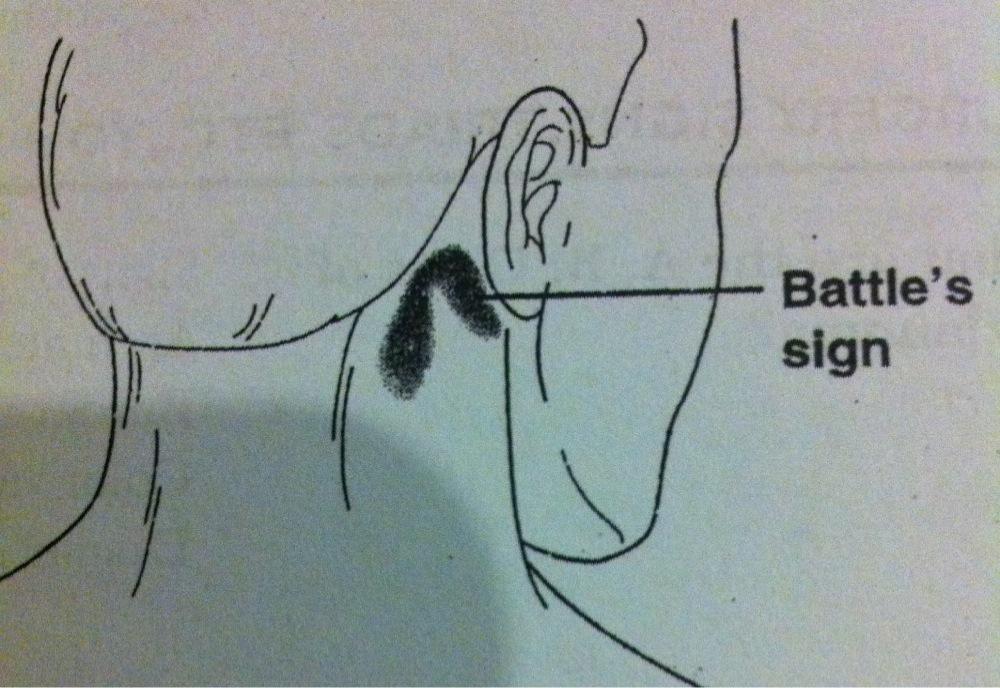
Battle sign presents as ecchymosis over the mastoid process, located behind the ear. It is typically associated with tenderness of the area as well. Other findings that may be seen that indicate basilar skull fracture include raccoon eyes (periorbital ecchymosis), hemotympanum (which is the presence of blood in the tympanic cavity of the middle ear), facial nerve injury, and laceration of the external auditory canal.
Battle sign is often present with a basilar skull fracture. The presence of Battle sign correlates with a positive predictive value of greater than 75% for the presence of an associated basilar skull fracture. In multiple studies, the Battle sign associated with a positive predictive value of 66% for intracranial lesions and 100% for skull base fractures.
Evaluation
Battle sign is a clinical sign. No further evaluation is needed to diagnose the sign. However, given that Battle sign correlates with an underlying skull fracture, imaging is typically warranted when Battle sign is observed. The initial evaluation is with a non-contrast computed tomogram (CT) scan, although linear or non-displaced fractures may not be detectable, necessitating further imaging. If the presentation gets delayed and infection is suspected, a contrast-enhanced CT or magnetic resonance imaging (MRI) may prove useful.
One must check for bleeding from the nose to rule out a CSF leak; this may be done by analyzing the presence of tau transferrin or glucose level.
Treatment / Management
In general, the treatment following skull fracture depends on the type of injury. Patients with linear fractures who have no neurological deficits and have a GCS of 14 or higher can be discharged home safely after a period of observation in the emergency room. However, the patient must be available for follow-up if he or she becomes symptomatic. Children with linear fractures need to be admitted overnight irrespective of the absence/presence of neurological deficits.
Surgery is usually required when patients have depressed skull fractures. The current consensus is that if the depressed segment is more than 5 mm below the inner table of adjacent bone, that the patient should undergo surgery to elevate that bone segment. Other indications for surgery include underlying hematoma, gross infection/contamination, and dural tear with pneumocephalus.
Patients should be treated with tetanus toxoid and broad-spectrum antibiotics if they have an open wound or if the presentation has been delayed.
Basilar skull fractures are secondary to trauma, and thus management requires a thorough trauma evaluation. Admission for observation is usually necessary, with further management determined based on the fracture.
Differential Diagnosis
Battle sign may be positive rarely in other conditions such as hepatic encephalopathy.
Prognosis
The Battle sign itself will fade and heal with time, although it may take several weeks for the ecchymosis to disappear. When Battle sign is present, the patient is more likely to have a slower than expected recovery from a head injury.
Complications
When patients present with Battle signs, it is vital to rule out associated cervical spine injury. Data reveal that 15% of patients with a basilar skull fracture have an associated cervical spine injury.
