Chemical Burns
Published (updated: ).

Healthcare professionals should be knowledgeable about chemical burns from exposure to acids (pH less than 7), alkalis (pH greater than 7), and irritants to recognize, manage and care for these common types of injury. Chemical burns are the result of exposure to a variety of substances commonly found in the home, workplace, and surrounding environment. The burn may be obvious, for example, from a direct spill or other exposure, or more covert, especially in children. Chemical burns can cause short-term, long-term, and lifelong health problems, especially if undertreated. Occasionally, they can result in premature death, especially if ingested in an attempt to self-harm.
Etiology
Chemical burns are the result of exposure to a variety of substances commonly found at home, the workplace, and the surrounding environment. The burn may be obvious, for example, from a direct spill or other exposure, or more covert, especially in children. Chemical burns can cause short-term, long-term, and lifelong health problems, especially if undertreated. Occasionally, they can result in premature death, especially if ingested in an attempt to self-harm.
Common causes of chemical burns include the following:
- Acids: Sulfuric, nitric, hydrofluoric, hydrochloric, acetic acid, formic, phosphoric, phenols, and chloroacetic acid
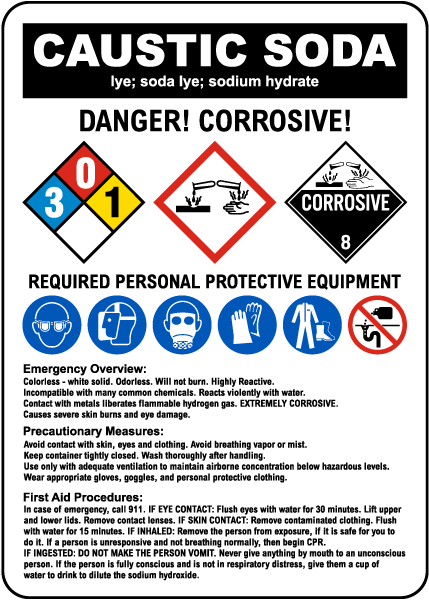
- Bases: Sodium and potassium hydroxide, calcium hydroxide, sodium and calcium hypochlorite, ammonia, phosphates, silicated, sodium carbonate, lithium hydride
- Oxidants: Bleaches like chlorites used in the home, peroxides, chromates, magnates
- Miscellaneous: White phosphorus, metals, hair coloring agents, airbag injuries
- Vesicants like mustard gas
Pathophysiology
Chemical burns cause damage as a result of irritant properties, acidity/alkalinity, concentration, form, amount of contact, the length of exposure, and location of contact. For example, contact with a mucosal surface such as the eye is likely to cause earlier and more extensive damage than contact with intact skin where there may be some barrier protection. After inadvertent or intentional ingestion, there will be prompt contact with the mucosal surface and both direct and absorptive toxicity.
Toxicokinetics
After exposure to an alkaline agent, the -OH moiety causes injury due to liquefaction necrosis, which leads to often irreversible changes in the protein matrix. Additionally, there is vascular damage that can create a local or systemic effect.
Acidic agents cause coagulation necrosis, which leads to cytotoxicity. Additionally, there are mucosal or skin changes that may prevent further toxicity and limit absorption. Overall, alkaline agents are more toxic than acidic agents, due to the irreversible changes in protein and tissue damage.
History and Physical
The most common findings represent structural changes to the tissue directly affected, for example, the eye, oral mucosa, skin, esophagus, and lower intestinal system, especially the stomach and pylorus, respiratory system, among others. In children, ingestion is generally the most worrisome event, because of changes, both short-term and long-term, often leading to extensive tissue death. Eye exposure, either acid or alkali, represents a significant acute injury. Copious irrigation is necessary, and measuring pH is appropriate, although rarely informative.
Evaluation
Direct examination of external exposure sites is mandatory, and if there is ingestion, endoscopic evaluation is necessary. In the instance of hydrofluoric (HF) acid exposure, monitoring of serum calcium and magnesium levels is critical to prevent chelation with the fluoride ion and cytotoxicity. With most other topical exposures, observation and serial monitoring of changes are sufficient.
Any gastrointestinal (GI) exposure must be seen by an experienced endoscopist who may need to perform serial evaluations to document healing. Likewise, eye injuries must be examined by an experienced ophthalmologist who will follow up with the patient sequentially and guide additional therapy.
With ingestions, especially when concerned about systemic absorption, laboratory evaluation (complete blood count [CBC], platelets, electrolytes, calcium, magnesium, arterial/venous blood gas, liver and kidney studies, lactic acid level, and, occasionally, coagulation studies) may be indicated. Radiographic studies, especially including an upright chest film, may help to determine if there is the presence of free air, which is suggestive of a perforation. Non-contrast CT may be used if there is concern about mediastinal free air, resulting from a perforation after exposure. Previously, a radio-opaque contrast was used, but this should be avoided in suspected perforation.
Treatment / Management
Copious irrigation of affected external areas is mandated. Endoscopic examination best explores internal injuries after ingestion. If there is concern about ingestion of disc or other flat batteries, radiographic assessment is mandated. It would be unusual that CT scanning would be needed, and MRI studies are interdicted. Ultrasonography in experienced hands may provide answers as to location as well.
It is not appropriate to introduce emetic agents or “neutralizing” agents into the treatment regimen after ingestion. There is high concern about aspiration, increased tissue damage with retching, and a strong possibility of exacerbating a bad situation. There is no current recommendation of systemic medications such as steroids, antibiotics, or prophylactic renal/hepatic therapies.

HF acid, among all the exposures mentioned above, can be treated with copious irrigation and application of a paste (commercially available and often supplied in an industrial setting where HF may be used commonly or made in the emergency department with powdered calcium gluconate and surgical lubricants). Some have recommended benzalkonium chloride solution. When applied, the treating clinician should use barrier protection. In some circumstances, intradermal or intraarterial injections of calcium (gluconate strongly preferred) have been used. Relief of pain is a good marker of the efficacy of treatment. Monitoring of calcium and magnesium levels is important. Oral ingestion, often in the context of suicidal behavior, is likely to be fatal and may be treated with lavage. Monitoring of heart rhythms and electrolytes, including calcium and magnesium, is necessary. Lavage may be helpful, especially if calcium salts are used.
Disc batteries have the potential to leak alkali and cause local, generally esophageal, burns. This is typically seen in children and will require endoscopic management and radiographic tracking of location. Early removal is strongly recommended. If the battery has passed the pylorus, watchful waiting, and inspection of stool for passage are appropriate.
