Cardiac Tamponade From Pericarditis
Published (updated: ).
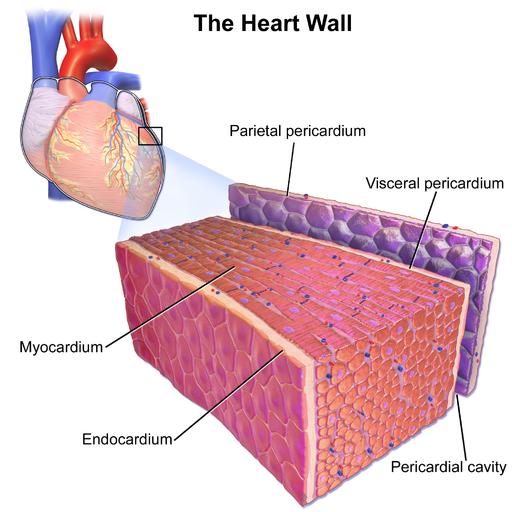
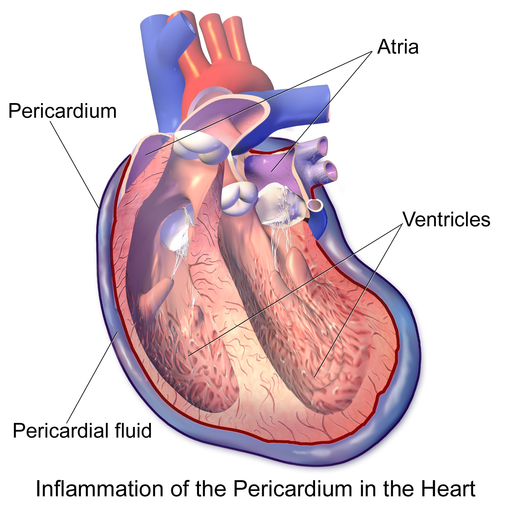
The pericardium is a membrane surrounding the heart. It comprises an outer fibrous pericardium and an inner double-layered serous pericardium. Serous pericardium includes visceral layer and parietal layers, separated by the pericardial cavity containing 15 to 50 ml of plasma ultra-filtrate in healthy people. The pericardium mechanically protects the heart. Pericardial diseases present as acute or chronic pericarditis, pericardial effusion, and cardiac tamponade. Pericarditis is a common disorder caused by inflammation of the pericardium. Acute pericarditis was reported in 5% of patients admitted to the emergency department and 0.1% to 0.2% of hospitalized patients for non-ischemic chest pain. Pericarditis can be divided into non-constructive and constrictive pericarditis. Pericarditis is commonly associated with pericardial effusion that can sometimes worsen to cardiac tamponade. Cardiac tamponade is a grave condition that happens after sudden and/or excessive accumulation of fluid in the pericardial space. The state restricts the appropriate filling of the cardiac chambers, disturbing normal hemodynamics, and ultimately causing hypotension and cardiac arrest.
Etiology
The cause of pericarditis is mostly idiopathic which makes up around 90% of cases. Other causes are infections caused by viruses, bacteria or tuberculosis. Other causes could include neoplasms, a connective tissue disorder, renal failure, post-myocardial infarction (also known as Dressler syndrome), open heart surgery (also known as the postpericardiotomy syndrome) and drugs, especially procainamide and hydralazine.
Cardiac tamponade may be caused by the accumulation of pericardial fluid from either a transudate, exudate, or blood. Slow accumulation such as in infections such as tuberculosis or myocarditis, autoimmune diseases, neoplasms, uremia, and other inflammatory diseases are better tolerated than rapid accumulation as seen in hemorrhages such as from a penetrating wound to the heart, ventricular wall rupture after myocardial infarction (MI) or following a pacemaker insertion complication.
Epidemiology
Acute pericarditis was reported in 0.1% to 0.2% of hospitalized patients for non-ischemic chest pain. The prevalence of pericardial effusions is difficult to estimate because a good deal of may not be clinically significant. The incidence or prevalence of pericardial effusions is estimated to be around 2 cases per 10,000 population. There is an increased prevalence in HIV-positive patients, end-stage renal disease, occult malignancies, tuberculosis, autoimmune diseases like lupus, or penetrating traumatic injury to the chest.
Pathophysiology
Pathophysiology includes infections, autoimmune process (Dressler syndrome, postpericardiotomy syndrome), uremia, connective tissue disorder. Most cases are idiopathic thought to be caused by a triggering of the inflammatory process resulting in inflammation of the pericardium which causes pericarditis.
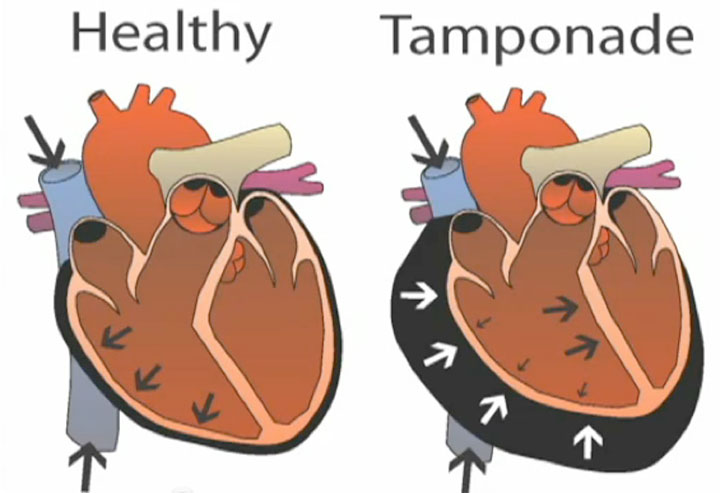
Cardiac tamponade results from the rapid filling of fluid within the pericardium, leading to compression of the chambers of the heart, further resulting in decreased venous return, ventricular filling and decreased cardiac output. Pericarditis, autoimmune diseases or neoplasms often result in slow-growing effusions, that over time become large before leading to cardiac tamponade type of picture.
History and Physical
Symptoms
Patients with pericarditis commonly present with sudden onset chest pain, which is pleuritic and classically improves when leaning forward and worsens when lying down. Patients with cardiac tamponade present with manifestations of cardiogenic or obstructive shock. They may endorse vague symptoms of chest pain, palpitations, shortness of breath, or in more severe cases, dizziness, syncope, and altered mental status. They may also present in a pulseless electrical activity cardiac arrest.
Signs
The classic physical findings in cardiac tamponade are included in Beck’s triad of hypotension, jugular venous distension, and muffled heart sounds. Pulses paradoxus, which is a decrease in systolic blood pressure by more than 10 mm Hg with inspiration is an important physical exam finding that suggests a pericardial effusion is causing cardiac tamponade. When fluid compresses the heart and impairs filling, the interventricular septum bows toward the left ventricle during inspiration due to increased venous return to the right side of the heart. This further decreases the left ventricle space leading to decreased left ventricular preload and stroke volume. The challenge with making the diagnosis of tamponade with clinical signs alone is difficult since they are neither sensitive nor specific.
Treatment / Management
Acute pericarditis often responds to treating the underlying cause. High-dose NSAIDs, with or without colchicine, tapered down over weeks is the first-line treatment. High dose aspirin (ASA) should be used in the post-myocardial infarction Dressler syndrome. The response is often assessed clinically based on symptom relief. Corticosteroids are not recommended as first-line therapy in most patients as it can increase the risk of recurrent pericarditis. Patients on the corticosteroid for recurrent pericarditis, steroid-sparing immunosuppressive agents (azathioprine or intravenous immunoglobulin) may be considered.
The treatment of cardiac tamponade is pericardiocentesis. During this procedure, a needle is advanced through the chest wall into the pericardium. The procedure may be done blindly or with guidance from ultrasonography or fluoroscopy. Hemodynamically unstable patients warrant the use of pericardiocentesis without imaging. Surgical drainage is required if the heart cannot be reached by a needle, clotted hemopericardium, intrapericardial bleeding, or thoracic conditions that make needle drainage difficult or ineffective. Definitive treatment to prevent further occurrence is achieved with a pericardial window, a surgical procedure performed by a cardiothoracic surgeon.
