Tension Pneumothorax
Published (updated: ).
Introduction
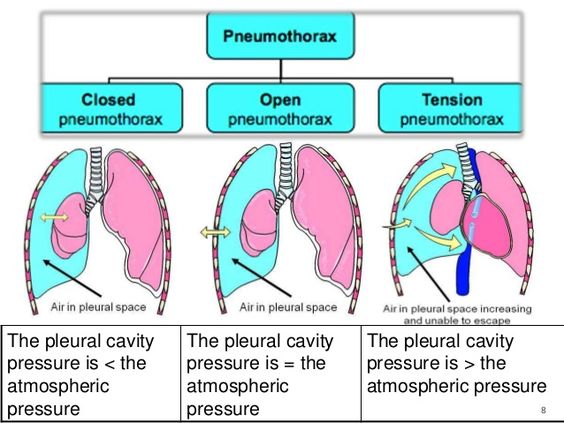
Pneumothorax is the collapse of the lung when air accumulates between the parietal and visceral pleura inside the chest. The air is outside the lung but inside the thoracic cavity. This places pressure on the lung and can lead to its collapse and a shift of the surrounding structures. Pneumothoraces can be traumatic or atraumatic. Traumatic pneumothoraces occur secondary to penetrating or blunt trauma, or they are iatrogenic. Iatrogenic pneumothorax is a traumatic pneumothorax that results from injury to the pleura, with air introduced into the pleural cavity secondary to a diagnostic or therapeutic medical intervention. Atraumatic pneumothoraces are further divided into primary (unknown etiology) and secondary (patient with an underlying pulmonary disease).
Pneumothoraces are classified as simple (no shift of mediastinal structures), tension (shift in mediastinal structures present), or open (air passing through an open chest wound). Tension pneumothorax is an uncommon condition with a malignant course that might result in death if left untreated. It is a severe condition that results when air is trapped in the pleural space under positive pressure, displacing mediastinal structures and compromising cardiopulmonary function. It is most commonly encountered in the prehospital, emergency department, and intensive therapy unit (ITU) settings.
Early recognition of this condition is life-saving both outside the hospital and in modern ITUs. Knowledge of necessary emergency thoracic decompression procedures is essential for all healthcare professionals. Traumatic and tension pneumothoraces are life-threatening and require immediate treatment.
Etiology
Causes of traumatic pneumothorax include the following:
Iatrogenic (induced by a medical procedure)
- Central venous catheterization in the subclavian or internal jugular vein
- Lung biopsy
- Barotrauma due to positive pressure ventilation
- Percutaneous tracheostomy
- Thoracentesis
- Pacemaker insertion
- Bronchoscopy
- Cardiopulmonary resuscitation
- Intercostal nerve block
Non-iatrogenic (due to external trauma)
- Penetrating or blunt trauma
- Rib fracture
- Diving or flying
Causes of tension pneumothorax:
All the above causes can further cause tension pneumothorax as well as:
- Idiopathic spontaneous pneumothorax
- Open pneumothorax
- Conversion of spontaneous pneumothorax to tension
Pathophysiology
Before understanding the pathophysiology of tension pneumothorax, it is essential to understand normal lung physiology. Pleural cavity (or intrapleural) pressure is negative as compared to lung pressure and atmospheric pressure. There is a tendency for the lung to recoil inward and the chest wall to recoil outward. That pressure gradient between the lung and pleural space prevents the lung from collapsing. During a pneumothorax, communication develops between the pleural space and the lung, resulting in air movement from the lung into the pleural space. This removes the pressure gradient usually present and causes a progressive rise in intrapleural pressure. This rise in pressure further compresses the lung and decreases its volume. The ipsilateral lung is unable to function at its normal capacity, and ventilation is then reduced, resulting in hypoxemia.
Tension pneumothorax occurs when the air enters the pleural space but cannot fully exit, similar to a one-way valve mechanism through the disrupted pleura or tracheobronchial tree. During inspiration, a sizeable high-pressure air collection accumulates in the intrapleural space and is not able to completely exit during expiration. This will cause the lung to collapse on the ipsilateral side. As the pressure increases, it will cause the mediastinum to shift towards the contralateral side, contributing further to hypoxemia. In severe cases, the increased pressure can also compress the heart, the contralateral lung, and the vasculature leading to hemodynamic instability and cardiac arrest in some cases. This is due to impaired cardiac filling and reduced venous return. Hypoxemia also triggers pulmonary vasoconstriction and increases pulmonary vascular resistance. As a result, hypoxemia, acidosis, and decreased cardiac output can lead to cardiac arrest and, ultimately, death if the tension pneumothorax is not managed in a timely fashion.
Traumatic pneumothorax occurs secondary to penetrating (e.g., gunshot wounds, stab wounds) or blunt chest trauma. Depending on the depth of a penetrating chest wound, the air will flow into the pleural space either through the chest wall or from the visceral pleura of the tracheobronchial tree. With blunt force trauma, a pneumothorax can occur if a rib fracture or dislocation lacerates the visceral pleura. An alternative mechanism is blunt thoracic trauma, where the increased alveolar pressure can cause the alveoli to rupture, resulting in the air entering the pleural cavity.
History and Physical
Patients with pneumothorax can be either asymptomatic or symptomatic. In a small pneumothorax, many patients may present without symptoms. However, tension pneumothorax is typically symptomatic, and its features are more impressive than spontaneous pneumothorax. Occasionally, it can have a subtle presentation too.
Symptomatic patients will present with sharp pleuritic pain that can radiate to the ipsilateral back or shoulder. The severely symptomatic patients will present with shortness of breath. Upon history taking, it is essential to note whether the patient previously had a pneumothorax, as recurrence is seen in more than 15% of cases on either the ipsilateral or contralateral side.
On examination, it is essential to assess for signs of respiratory distress, including increased respiratory rate, dyspnea, and retractions. On lung auscultation, decreased or absent breath sounds on the ipsilateral side, reduced tactile fremitus, hyper-resonant percussion sounds, and possible asymmetrical lung expansion are suggestive of pneumothorax. With tension pneumothorax, patients will have signs of hemodynamic instability with hypotension and tachycardia. Cyanosis and jugular venous distension can also be present. In severe cases, or if the diagnosis was missed, patients could develop acute respiratory failure and possibly cardiac arrest. In some instances, subcutaneous emphysema can also be seen. The diagnosis of tension pneumothorax must be made immediately through clinical assessment as waiting for imaging, if not readily available, may delay management and increase mortality.
Treatment / Management
Tension pneumothorax can occur anywhere, and treatment depends on the circumstance at the time of onset. It is usually managed in the emergency department or the intensive care unit. Management strategies depend on the hemodynamic stability of the patient. In any patient presenting with chest trauma, airway, breathing, and circulation should be assessed. Penetrating chest wounds must be covered with an airtight occlusive bandage and clean plastic sheeting. Administration of 100% supplemental oxygen can help reduce the size of the pneumothorax by decreasing the alveolar nitrogen partial pressure. This creates a diffusion gradient for nitrogen, thus accelerating the resolution of the pneumothorax. Only 1.25% of the air is absorbed without oxygen in 24 hours. Positive pressure ventilation should be avoided initially, as it will increase the tension pneumothorax’s size. Patients can be placed on positive pressure ventilation after a chest tube is placed.
If the patient is hemodynamically unstable and clinical suspicion is high for pneumothorax, immediate needle decompression must be performed without delay. Needle decompression is done at the second intercostal space in the midclavicular line above the rib with an angio-catheter. It results in the re-expansion of the collapsed lung. However, the risk of lung re-expanding quickly increases the risk of pulmonary edema. Following needle decompression, a CXR is done, and a chest tube is usually placed.
Assessment of pneumothorax resolution is usually done with serial chest X-rays. Then, when the patient has improved, the lung has fully expanded, and no air leaks are visible, the chest tube is ready to be removed.
