Spontaneous Pneumothorax
Published (updated: ).
Introduction
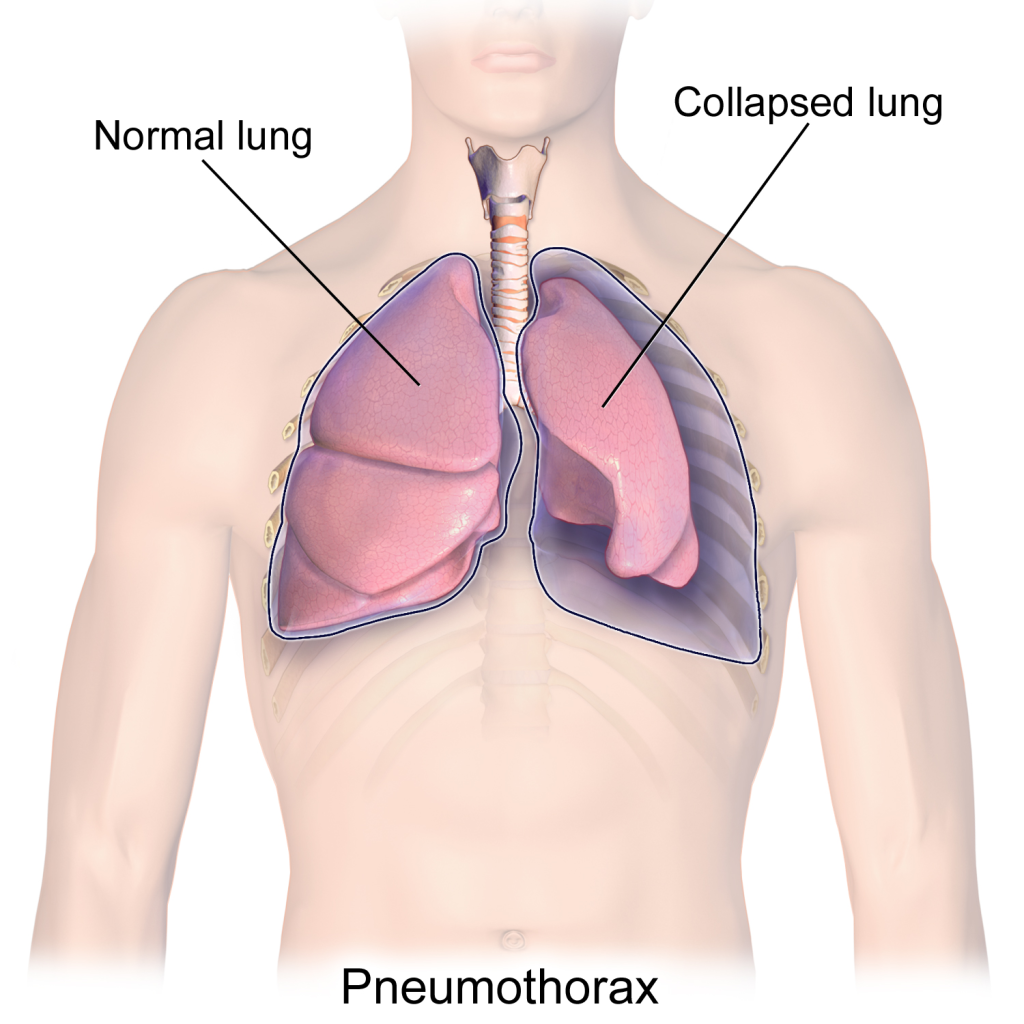
Spontaneous pneumothorax refers to the abnormal collection of gas in the pleural space between the lungs and the chest wall. Spontaneous pneumothorax occurs without an obvious etiology such as trauma or iatrogenic causes. Spontaneous pneumothorax can be classified as either primary or secondary. Primary spontaneous pneumothorax (PSP) occurs when the patient does not have a history of the underlying pulmonary disease, whereas secondary spontaneous pneumothorax (SSP) is associated with a history of an underlying pulmonary disease. Patients may present with a variety of symptoms including tachycardia and dyspnea. A feared complication is tension pneumothorax. The diagnosis of spontaneous pneumothorax is based on clinical suspicion and can be confirmed with imaging. Management of spontaneous pneumothorax depends on multiple factors including the patient’s stability, the size of the pneumothorax, occurrence (i.e., first episode or recurrent), and the type of spontaneous pneumothorax (i.e., primary spontaneous pneumothorax or secondary spontaneous pneumothorax).
Etiology
While primary spontaneous pneumothorax is not associated with underlying pulmonary disease, secondary spontaneous pneumothorax is associated with, but not limited to, the following:
- Chronic obstructive pulmonary disease
- Asthma
- Cystic fibrosis
- Pneumonia (e.g., necrotizing, Pneumocystis jirovecii)
- Pulmonary abscess
- Tuberculosis
- Malignancy
- Interstitial lung disease (e.g., idiopathic pulmonary fibrosis, sarcoidosis, lymphangioleiomyomatosis)
- Connective tissue disease (e.g., Marfan syndrome, Ehlers-Danlos syndrome, rheumatoid arthritis)
- Pulmonary infarct
- Foreign body aspiration
- Catamenial (i.e., associated with menses secondary to thoracic endometriosis)
- Birt-Hogg-Dube syndrome
Pathophysiology
The main principle of the pathophysiology of spontaneous pneumothorax revolves around gas leaking into the pleural space. Spontaneous pneumothorax is a multifactorial process and has been associated with rises in transpulmonary pressure and defects in the visceral pleura. Acute increases in alveolar pressure that exceed the pulmonary interstitial pressure can lead to alveolar rupture and pleural air leakage. Furthermore, points of weakness in the visceral pleura due to subpleural blebs, bullae, lung necrosis, and other connective tissue abnormalities can predispose the alveoli to rupture in both types of spontaneous pneumothorax, though the exact mechanism of how is not entirely understood. Intact bullae without an explicit defect in the visceral pleura have been shown to be associated with spontaneous pneumothorax; however, histopathological analyses and scanning electron microscopic studies of tissue obtained from thoracotomies suggest that sloughing of pleural mesothelial cells may play a significant role in the development of spontaneous pneumothorax.
History and Physical
Spontaneous pneumothorax most commonly occurs at rest without a history of an exertional component. Patients are often complaining of sharp, pleuritic ipsilateral chest pain or acute dyspnea and increased work of breathing, especially patients with secondary spontaneous pneumothorax. Tachycardia is one of the most common physical exam findings; however, in patients with smaller spontaneous pneumothorax (less than 15% of the hemithorax), the exam may be unremarkable. For patients with larger spontaneous pneumothorax (more than 15%), there may be reduced movement of the chest wall, ipsilateral decreased or absent breath sounds, jugular venous distension, pulsus paradoxus, hyperresonance on percussion, and decreased tactile fremitus. Development of a tension pneumothorax is a rare potential complication of spontaneous pneumothorax with the late, ominous findings of hypoxemia, hypotension, and tracheal deviation.
Evaluation
The diagnosis of spontaneous pneumothorax is often suggested by the patient’s history and physical exam findings, which can be confirmed by imaging. Chest radiography characteristically shows the displacement of the visceral pleural line with a space devoid of lung markings in between. While upright films are preferred, there is evidence that expiration does not necessarily increase the diagnostic yield. Ultrasound has also shown diagnostic potential. There is evidence that ultrasound has greater sensitivity than chest radiography; however, both modalities are limited in how well they estimate the size of a pneumothorax. The use of chest computed tomography (CT) for the diagnosis of spontaneous pneumothorax has been debated. The high sensitivity and specificity of CT can be of value when there is a high index of suspicion for spontaneous pneumothorax, and initial imaging is negative or equivocal. While arterial-blood gas measurements are not necessary for a diagnosis of spontaneous pneumothorax, they can be useful in assessing acute respiratory alkalosis and increases in the alveolar-arterial oxygen gradient when tension physiology is present.
