Pneumothorax
Published (updated: ).
Introduction
Traumatic pneumothorax is the second most common injury in chest trauma, accounting for 50,000 cases a year in the United States. Pneumothorax management relies on early recognition and treatment by prehospital providers to prevent the development of respiratory failure or obstructive shock from “tension” physiology. The majority of emergency medical service (EMS) providers in the United States have protocols for rapid assessment and treatment of pneumothorax. There are multiple treatment modalities available for use by prehospital providers with varying use by both levels of training and geographic location. No single accepted method is being performed on a national level.
Anatomy and Physiology
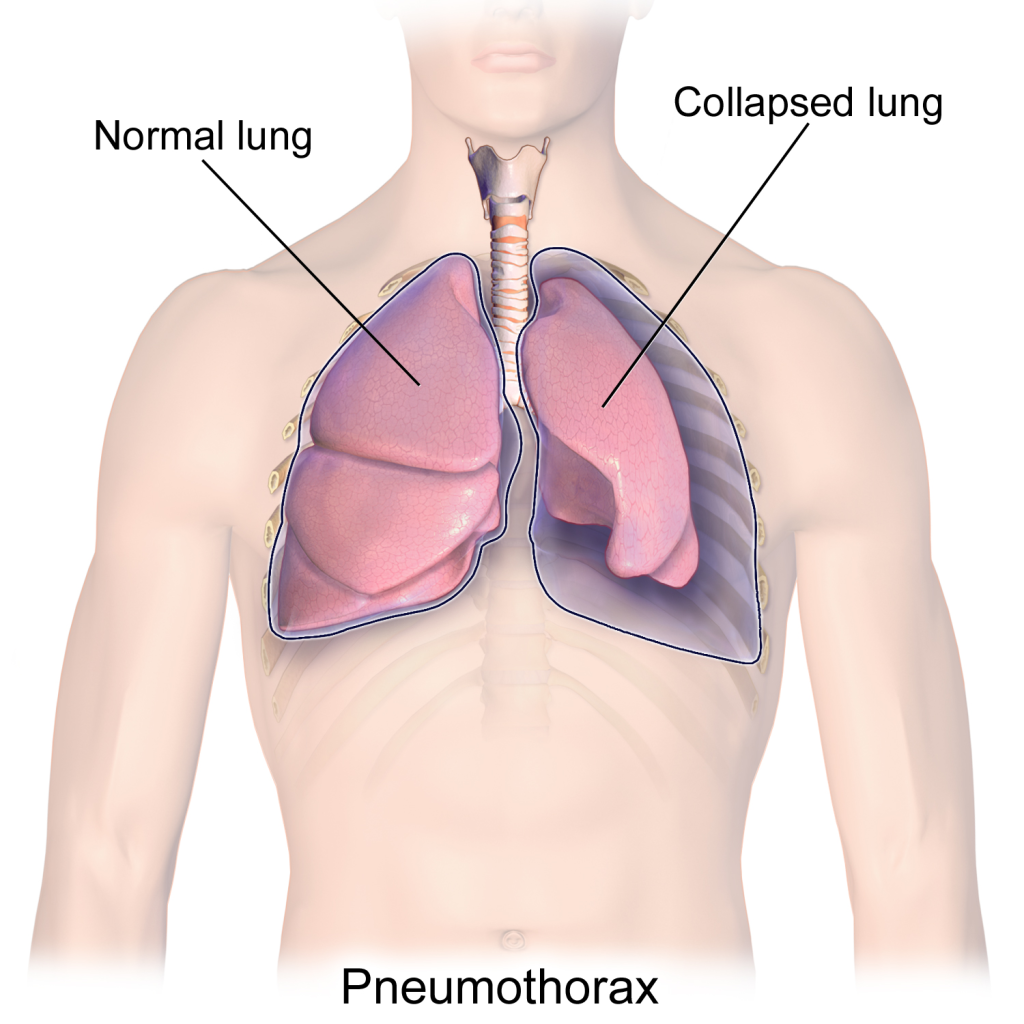
The pleural space and the neighboring tissues are important to understanding the pathophysiology of traumatic pneumothorax. The potential space between the visceral pleural lining and the parietal pleural lining is normally one that allows for movement of tissue without occupying a large area within the thorax. When this space is violated from trauma, blood and air can enter this potential space. The increasing pressure in this space results in various pathologies. This increased area of pressure then exerts its effects on the surrounding tissues. This interference will lead to changes in normal intrathoracic pressure which can hinder blood flow and ventilation to the thorax.
Three broad classes of traumatic pneumothorax are simple, tension, and communicating. Simple pneumothorax occurs due to the injury to the lining of the lung or pleura that allows for the accumulation of air in that pleural space. The majority of these occur in the setting of blunt trauma. The blunt force results in broken ribs that can injure the pleura or lung tissue itself. This direct injury will allow air to enter into the potential space between the parietal and visceral pleura. The presence of air will not cause effects to the neighboring structures unless a large amount of air and pressure accumulate.
Tension pneumothorax can be thought of as a continuum of the simple pneumothorax. Tension pneumothorax occurs when a large accumulation of air in the pleural space leads to the increased thoracic pressure that results in compression of other thoracic structures. This effect on the pulmonary tissues will lead to the collapse of the lung which causes diminished ventilation and oxygenation as the normal intrathoracic negative pressure used for ventilation becomes compromised. Compression of the vasculature from the displacement by the pneumothorax will cause decreased venous return and a drop in cardiac output. This resistance to blood flow results in obstructive shock with tachycardia and eventual hypotension and, if left untreated, can result in cardiac arrest.
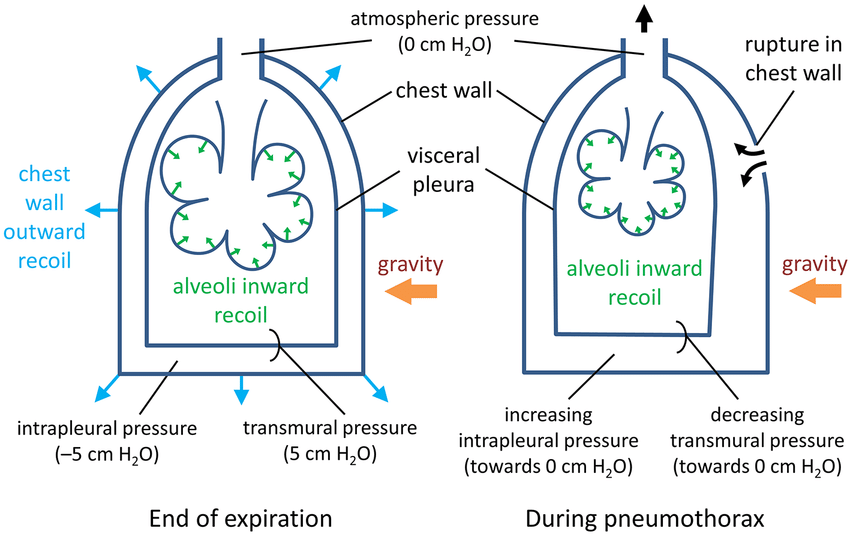
Open or communicating pneumothorax is the result of a penetrating injury through the chest wall which allows for communication of air between the atmosphere and the potential pleural space. This leads to dysfunction when negative pressure forces produced during thoracic cavity expansion allow for air to enter the pleural space. Instead of the normal negative pressure inside the thorax that is essential for ventilation, atmospheric pressure develops and impedes air movement. Unlike the simple pneumothorax, the open pneumothorax cannot lead to tension physiology as the open communication allows for air to escape when pressure builds beyond atmospheric pressure. Due to the effects of inspiration, this injury still can lead to respiratory failure unless corrected
Indications
Pneumothorax should be considered in the setting of thoracic trauma where there are clinical signs of respiratory or circulatory compromise. Classically the findings of hypoxia, chest wall crepitus, diminished breath sounds, tachypnea, tachycardia, hypotension, tracheal deviation, and the presence of a sucking chest wound all have been used to help make the diagnosis. Many of these findings are observed in the primary survey of the trauma patient and can be obtained by the prehospital provider. It is paramount to note that some of these findings, which are used in protocolized guidelines of treatment, are somewhat unreliable and may only be late findings.
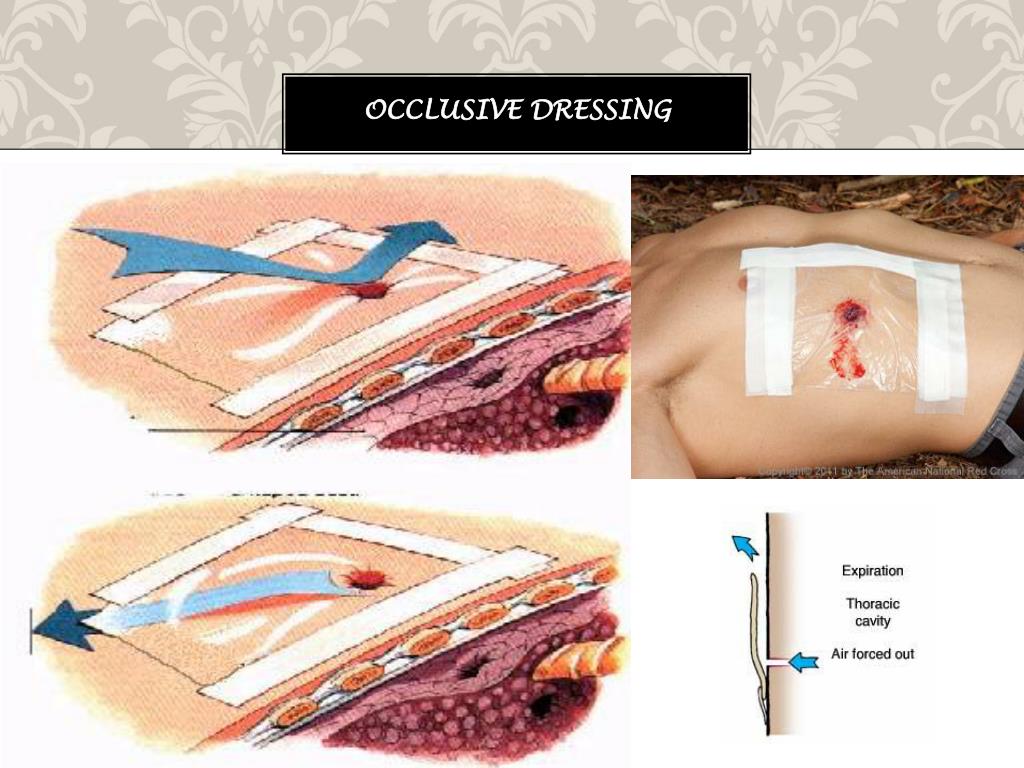
Two main procedures are used in the emergency management of pneumothorax in the prehospital setting: needle thoracostomy for tension pneumothorax and the placement of three-sided occlusive dressing for a communicating pneumothorax. The presence of thoracic trauma, absent or diminished breath sounds on auscultation, and significant hypotension and or hypoxia/respiratory failure should prompt a provider to consider needle thoracostomy to relieve suspected tension pneumothorax. Practitioners should also consider the environment of the communicating pneumothorax that has been addressed with an occlusive dressing. Although there may have been a communicating wound before treatment, once an occlusive dressing is applied, the pneumothorax can develop tension physiology.
The presence of a sucking chest wound on physical examination should prompt the provider to consider treatment for a communicating pneumothorax. The placement of an occlusive dressing is indicated in this setting, regardless of respiratory status, given the propensity for these patients to deteriorate and the innocuous nature of the dressing placement. If there is no sign of respiratory compromise and the patient is otherwise asymptomatic, consideration of rapid transport over dressing placement is at the discretion of the prehospital provider.
Contraindications
There are no absolute contraindications for treatment of tension pneumothorax with needle thoracostomy or treatment of communicating pneumothorax with an occlusive dressing. The overall condition of the patient, time to transport to a facility, and other patient-specific factors such as chronic anticoagulation can help the practitioner make the decision of whether to pursue more invasive measures or delay therapy to more definitive treatment such as thoracostomy in the hospital setting. Ultimately, given the high morbidity and mortality associated with these injuries, the treatment is often necessary and should not be delayed in the unstable patient for any of these factors.
Equipment
The best equipment to use for the treatment of tension pneumothorax with needle thoracostomy has been hotly debated. Various prehospital providers use commercial devices and traditional angiocatheters. Considerations for cost and efficacy of these various modalities have yet to yield one definitive national standard. One of the biggest concerns that have been studied has been the success rate of needle thoracostomy and which approach yields the highest success rate. Due to the evergrowing body mass index of patient populations, an increasing number of EMS systems are adopting larger bore and longer devices to combat the distance needed to penetrate the pleural space. Additional studies also have advocated for different areas of needle placement which will be discussed below. The prehospital provider should be familiar with the available equipment and its use.
Classically three-sided occlusive dressings were placed to relieve communicating pneumothorax. Concerns about the time required to place the dressing and difficulty with properly taping it to the chest have led to the development of other techniques and commercially available devices. Other devices that have been developed include occlusive devices with valves, suction ports, and ventilated tracts. To date, no randomized control trials on humans have been done to compare these devices, but multiple studies have been done in porcine models. Of the devices tested the most effective were linear ventilated occlusive dressings as they were less likely to be clogged with blood clots and were better at adhering to the patient than traditional methods of tape. The cost of these engineered ventilated dressings is substantial compared to simple occlusive dressing with tape, and the prehospital provider should be familiar with the available equipment and its use within their system.
Personnel
Both of these procedures are in the scope of practice of any prehospital provider with the equipment present to perform the procedure. The majority of prehospital systems should have protocols in place for who can perform these procedures and when they should be performed. Provider familiarity with these protocols is paramount.
With ever-improving technology, there may be roles for in-hospital approaches to be adapted to the prehospital setting to improve diagnostic accuracy as well as improve time to diagnosis. Ultrasound has been demonstrated many times in the emergency department literature to be a quick and effective tool in the rapid diagnosis of pneumothorax and is now considered part of the standard approach to the traumatically injured patient. What was once a large, cumbersome technology is rapidly becoming more portable and accessible and perhaps a future tool in the arsenal of prehospital workers. Ultrasound probes can connect to portable electronic devices, allowing for a mobile tool to be used in the field to help assess patients. In time this may become the new standard of care for prehospital providers, but more research will be needed to demonstrate the effect on patient outcomes.
Preparation
The approach to any patient with suspected pneumothorax is to prevent further tension physiology to develop and support the patient’s ventilation. Patients can benefit from supplemental oxygen use which helps with both oxygenation and pneumothorax reabsorption. Pain control should be given for suspected rib injuries which may cause splinting and decrease the patient’s ability to ventilate. If shock is present, evaluation and treatment of other causes should not be avoided, even if a pneumothorax is suspected, as often multiple sources of shock may be present in the traumatically injured patient. Lastly, avoid positive pressure ventilation unless it is necessary due to respiratory failure. Ultimately the EMS provider must be constantly vigilant in the identification of developing tension physiology and be ready to intervene with decompression if necessary.
Rapid exposure and assessment of the chest wall in the setting of a penetrating chest injury can identify sucking chest wounds. Additional attention should be paid to the axilla and posterior back where these wounds may not be readily seen in the supine patient. Because the most frequently seen complication with occlusive dressing application is difficulty in keeping it on the patient, remove moisture from the application area before placement when possible.
Technique

Needle decompression is done by placing a large-bore catheter through the chest wall into the pleural space and allowing for the release of pleural air. Identification of landmarks is done via palpation and visualization with the goal to place the needle just above the rib to avoid the larger blood vessels of the chest wall. Many cases document an audible whoosh of air leaving the catheter that was placed properly, but this may not occur with every placement. Instead, improvement of vital signs is often seen as a sign of successful placement.
The procedure for dressing a sucking chest wound aims to prevent any further communication of air with the pleural space and is achieved with placement of an occlusive dressing with the goal of allowing for a one-way valve over the wound. The result should be a device that allows air to leave the pleural space without allowing for backflow of air with inspiration. Classically, an occlusive dressing is applied and adhered to the chest on three sides with the dependent portion open to allow for blood and air to escape the wound. Commercial devices work similarly but are designed to be adherent and allow for drainage and are simply applied over the wound. In the military setting, they have elected to eliminate the three-sided dressing altogether and instead recommend a complete four-sided occlusive dressing with needle decompression if tension physiology were to develop.
Complications
The complications associated with occlusive dressings are less a product of the procedure and more of a failure for the procedure to achieve an effective one-way flap over the wound. The most common complications are a loss of adherence to the patient, resulting in a continued communicating pneumothorax, or occlusion of the wound itself, resulting in a closed pneumothorax with the potential to develop tension physiology. The often concomitant hemothorax associated with these injuries furthers the likelihood of either of these possibilities as bleeding may hinder adherence of the dressing to the chest wall and clotted blood may obstruct the tract preventing pleural air to escape the thoracic cavity. Additional complications are rarely life-threatening, but localized allergic reactions have been reported with some adhesives.
