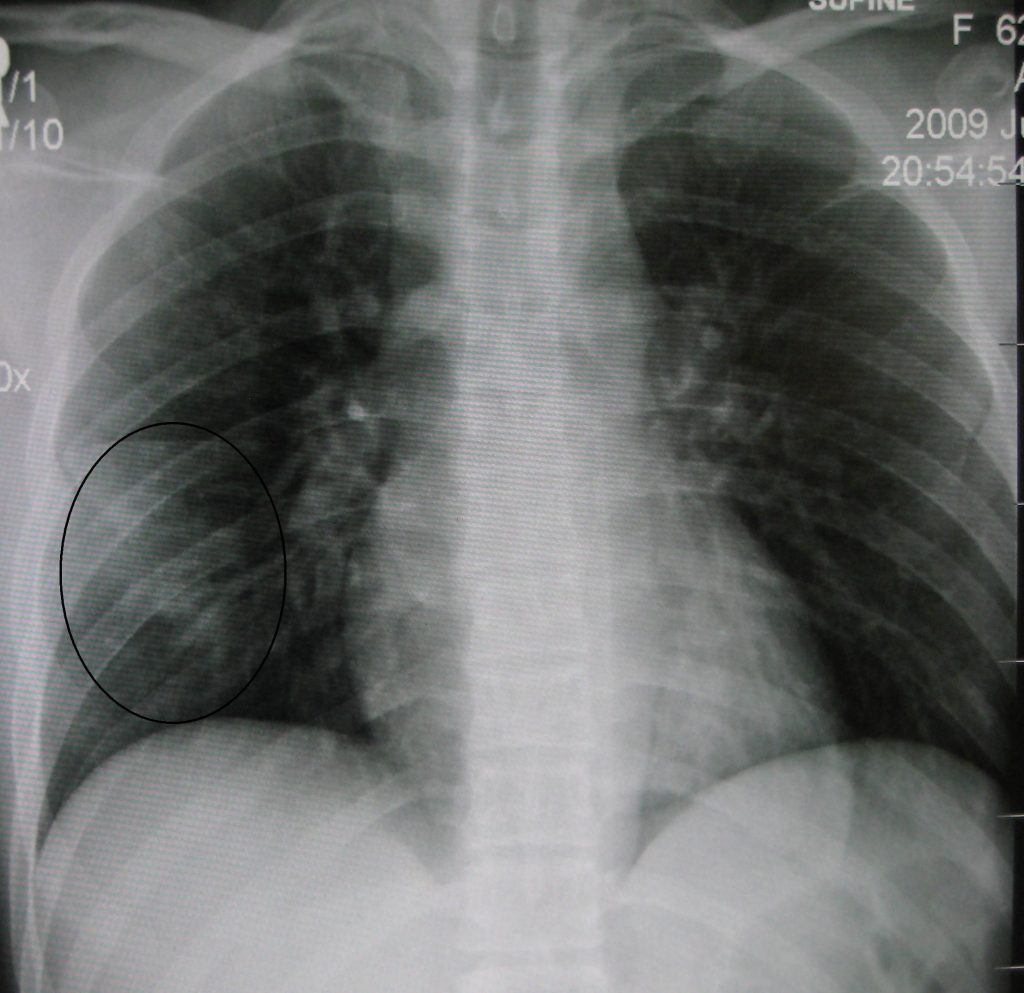
Pulmonary Contusion
Published .
A pulmonary contusion is an injury to the lung parenchyma in the absence of laceration to lung tissue or any vascular structures. It usually results from blunt chest trauma, shock waves associated with penetrating chest injury, or explosion injuries. These injuries can lead to pulmonary failure and death. The pathophysiology of pulmonary contusions remains poorly understood. Widespread use of explosives at World War 1 and 2 led to increased recognition of pulmonary contusion due to blast injuries. Many soldiers with blast injuries developed pulmonary bleeding without apparent external injuries.
Any chest trauma, blunt, penetrating, or a combination of both, can lead to a pulmonary contusion. Explosions falls from great heights, and sports injuries are other identified causes. A pulmonary contusion is the most commonly identified lung injury (30% to 75%) in blunt chest traumas, with a mortality rate of 10-25%. Children have more flexible chest bones, resulting in large forces transmitted to the lung tissue and significantly more severe contusions without apparent external injuries after blunt chest trauma.
Pathophysiology
A pulmonary contusion causes injury to the lung parenchymal, leading to disruption of alveoli and capillaries, resulting in leakage of blood and other interstitial fluids (water and serum) across the alveolar-capillary membrane into lung tissue and alveolar space. Fluid in the alveolar space leads to alveolar edema and a decrease in the amount of surfactant, leading to alveolar collapse and atelectasis. Decreased lung compliance, ventilation-perfusion mismatch, and intra-pulmonary shunting result from the discoloration. Ventilation of the affected lung is impaired as oxygenated air can not enter fluid-filled alveoli during inspiration leading to reflex vasoconstriction and decreased perfusion, resulting in hypoxemia and hypercapnia.
Lung injury due to pulmonary contusion leads to activation of the immune system, resulting in tissue macrophage activation, accumulation of blood leucocytes, and increased production of cytokines, chemokines, arachidonic acid metabolites, oxygen radicals, complement, and coagulation cascades. The resulting increased inflammatory response causes impaired neutrophilic apoptosis and increased alveolar epithelial apoptosis. Severe inflammation may cause Acute Respiratory Distress Syndrome (ARDS). The contralateral intact chest may be involved, resulting in edema and inflammation.
Concurrent aspiration of gastric acid can complicate a pulmonary contusion by worsening the permeability of lung injury and increasing inflammatory response and progress to ARDS and pneumonia.
Three possible mechanisms are suggested for resulting in pulmonary contusion.
- The spalling effect leads to increased cell membrane permeability due to the interruption of the lipid layer when a pressure wave encounters a liquid-gas interface, such as the alveolar wall.
- The inertial effect, when a pressure wave encounters tissues with different densities, leads to a different rate of acceleration and deceleration, resulting in lighter alveoli stripping away from denser bronchial tissue.
- Implosion effect, when a pressure wave encounters tissues with air bubbles, compresses the gas within tissues, and a rebound leads to stretching and tearing of tissues due to over-expansion.
Histopathology
Pulmonary hemorrhage may be associated with pulmonary contusion. Alveolar or interstitial fluid accumulation was found on biopsy in soldiers during world war 2, initially attributed to fluid resuscitation. In recent years animal models of disease have identified interstitial hemorrhage followed by edema and inflammatory cell infiltration.
History and Physical
Based on the severity of pulmonary contusion and other concurrent injuries, the clinical presentation may vary. It may present with difficulty breathing and coughing, whereas mild cases may be asymptomatic. The affected area of the chest may be tender. Breath sounds may be decreased on auscultation. In severe cases, hemoptysis may be the presenting symptom. In extreme cases, alveolar gas exchange is disrupted, resulting in hypoxemia and hypercarbia, which leads to tachypnea and dyspnea.
In severe contusion, symptoms appear within hours, whereas in mild injury, symptoms may develop gradually over 24-48 hrs.
Complications
Pulmonary contusions may result in respiratory failure, progress to ARDS, and pneumonia. Patients with polytrauma are more likely (78%) to develop ARDS than those with only pulmonary contusions (17%).
