Communication: One Size Does Not Necessarily Fit All
Published .
It is important for the EMT to remember that if the right questions are asked, the patient may just be able to tell the ambulance crew what is wrong. The vast majority of time, the patient absolutely knows what is wrong; all the EMT needs to do is ask.
When addressing older patients (at least in Georgia), the EMT should be polite, address the patient by their last name preceded by Mr. or Mrs. Georgians are expected to respect their elders. When the EMT and the patient are the same age, it is appropriate to address the patient by their first name. If the patient is a Judge, Doctor or somebody that has a special title, it is acceptable to call them by their elected name.
How a patient will respond to an EMT can be a function of the patient’s age. An infant will not really be bothered by the EMT so long as the infant is near the parent or caregiver (separation anxiety). A toddler will not want the EMT to even be in the same room as them (stranger anxiety). Clearly, when treating infants or toddlers, the EMT would be wise to enlist the help of the parent or caregiver. All patients respond to respect and need to understand that the EMT is here to help.
Don’t Be Ashamed, Be Helpful
The EMT should introduce him/herself to the patient in whatever way they would like to be addressed. “My name is Gary and I am a Paramedic, I am here to help; what brings us to your house today Mr. Smith.” The EMT needs to remember that they bring themselves to the call and the EMT should just try to be who they are when addressing a patient. In Georgia, many people have pronounced southern dialects. Many patients are from the northeastern United States. Many people from the northeast think that a southern drawl is a sign of ignorance. It is generally considered inappropriate for an EMT to emulate the characteristics of the people they are serving. Issues like this are typically referred to as a cultural bias. Cultural differences between Americans are not a profound as patients from other countries. In some middle eastern cultures, it is inappropriate for a male EMT to speak to, much less assess a female patient. This situation can be extremely frustrating if the call happens to be an obstetric call.
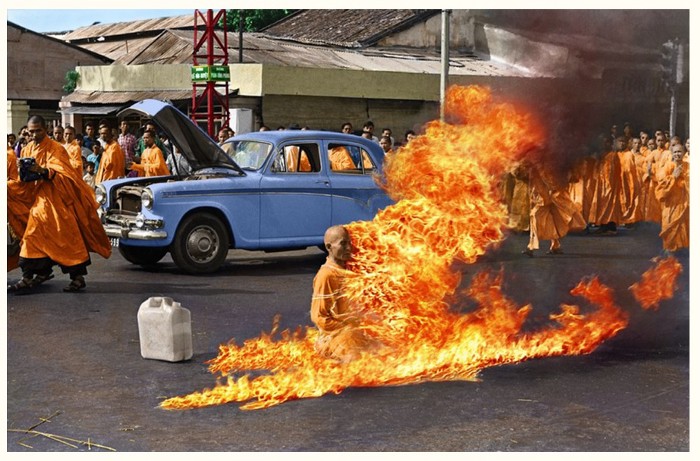
Aside from basic communication, the position of the EMT may be enough to put the patient in a compromising situation in regards to their beliefs. Let’s say a patient cuts himself in the kitchen, the bleeding is controlled, and possibly will require suturing. The EMS crew offers to transport the patient to the hospital but the patient refuses on the basis that the hospital will want to give the patient a tetanus shot. Some cultures do not practice vaccination. Some religions won’t allow a patient to receive a blood transfusion. These are all examples of ethnocentrism. The patient places the EMS crew in a cultural imposition ( the tendency of an individual or a group to believe that their cultural values and beliefs should be dominant).
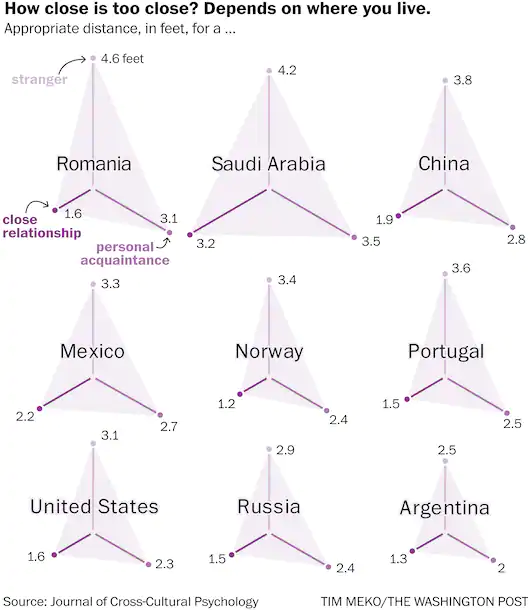
Body space is a function of who a patient or caregiver is outside of the ambulance. There are differences in opinion based on where people are from geographically that define what appropriate body space should be. In the world of body space, there are multiple zones:
- Intimate zone – touching zone
- Personal distance – Interactions between good friends or family. 1.5 – 4.5 feet away depending upon how well the people know each other
- Social distance – Interactions among acquaintances; 4 – 12 feet away
- Public Distance – Public speaking distance; greater 12 feet away.
When working with patients from other countries, the patient may take the sick role completely different than an American. Some cultures do not emote when they are in discomfort while others turn suffering into something everyone must experience. Nonverbal communication such as eye contact may be taken as aggressive or impolite in some cultures, where Americans tend to think that eye contact and a strong handshake are traits of the trustworthy. Without exception and despite Nation of Origin. The EMT should always ensure the patient has given permission to touch or examine the patient.
When confronted with a language barrier, the EMS agency should have a way to connect EMT’s with a translator service. A translator usually can speak to the patient over a cell phone and advise the EMS crew on what they patient is trying to say. Language lines are excellent services when the EMT has some idea as to what language the patient is speaking. Other times, bystanders or family members can be translators for the EMS crew. Sometimes, the patient doesn’t speak a different language, they are just deaf. The easiest way to communicate with a deaf person is to get a piece of paper and write your questions on the paper and have the patient respond on paper (rather time consuming and requires some patience).
