Spinal Shock
Published (updated: ).
Introduction
Spinal cord injury (SCI) is a common injury occurring in the United States with an incidence of approximately 54 per million persons per year. According to the National Spinal Cord Injury Statistical Center, approximately 280,000 living survivors of traumatic SCI were reported in the United States in 2017. The prevalence of nontraumatic SCI is unknown, but it is thought to be three to four times greater. Causes of spinal cord injury are diverse. Although trauma is the most common cause, other etiologies include myelopathies induced by autoimmune, infectious, neoplastic, vascular, and hereditary-degenerative diseases.
Acute traumatic SCI requires high-impact, direct trauma that leads to spinal cord injury and spinal shock. The initial encounter with a patient with spinal shock is usually under a trauma scenario. Ischemia of the spinal cord can also produce a spinal shock; for example, a hypotensive patient in the medical intensive care unit (ICU) or a post-angiography patient with thrombotic occlusion of arteries that supply the cervical spine can have a similar presentation. Treatment of ischemic spinal shock is different, and outcome expectations are also different. Cord injury is often associated with fracture-dislocation, tearing of ligaments, rotational distraction, as well as tearing of the disc space. If the spinal shock is not associated with significant injury of the spinal column itself, then the prognosis for these patients is more favorable than when a fracture is present. The overall treatment of patients with significant spinal shock and injury is a challenge, but aggressive medical management can reduce its effect on the overall functionality of the patient.
Etiology
Traffic accidents involving motor vehicles, bicycles, or pedestrians account for approximately 50% of all SCIs. In patients older than 65 years of age, domestic accidents such as falls are the most common cause of SCIs. Primary spinal cord injury may be due to transection of the cord, mechanical injury, abscess formation, or metastatic disease. Secondary spinal cord injuries may be due to occlusion or disruption of arterial blood supply to the spinal cord with resultant hypoperfusion and anoxic damage to the spinal cord.
Epidemiology
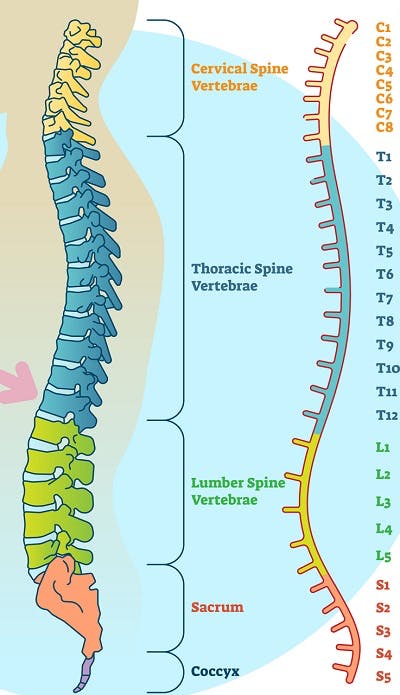
The worldwide annual incidence of spinal cord injury is reported to be around 15 to 40 cases per million. The majority of these cases are young men and have SCI secondary to trauma. Approximately 55% of acute SCIs occur in the cervical region. Cervical spine SCI has a worse prognosis compared to SCI of other spinal levels, which is reflected in the decreased prevalence of cervical SCI in epidemiologic data. In the United States, the National Spinal Cord Injury Statistical Center reported an incidence of 54 cases per one million people, equivalent to around 17,900 new SCI cases each year.
Pathophysiology
Acute SCI is a two-step process involving primary and secondary mechanisms. Primary injury occurs as a combination of initial impact with underlying chronic cord compression. This can occur with fracture-dislocation, burst fractures, and acutely ruptured discs. In some cases, primary injury can occur without pre-existing cord compression. This is seen with severe ligamentous injuries leading to transient spinal column dislocation or spinal cord laceration from sharp bone/metal. Mechanisms of secondary injury include inflammation, calcium-mediated mechanisms, sodium, glutamatergic pathways, vascular mechanisms, free radicals, and apoptosis.
History and Physical
It is important to familiarize oneself with the definitions of spinal shock and neurogenic shock. Although they are distinct entities, they are seen as a spectrum of the same disease process in patients with SCI (usually traumatic).
Spinal shock is the altered physiologic state immediately after a spinal cord injury (SCI), which presents as loss of spinal cord function caudal to the level of the injury, with flaccid paralysis, anesthesia, absent bowel and bladder control, and loss of reflex activity.
Neurogenic shock is a component of the spinal shock syndrome and refers to the hemodynamic instability seen in these patients with hypotension, bradycardia, and hypothermia (secondary to sympathetic-parasympathetic dysfunction/imbalance).
Evaluation
The primary assessment of a patient with trauma and possible underlying spinal shock includes evaluation of airway, breathing, and circulation. Care should be taken to ensure movement of the spine does not occur to minimize secondary injury. The patient should be immobilized at the scene and during transport. A rigid cervical collar and supportive blocks on a backboard with straps are recommended. The movement of the patient should be done using the log-roll technique. If mechanical ventilation is necessary on an emergent basis, rapid-sequence intubation with in-line spinal immobilization can be used; however, intubation over a flexible fiberoptic laryngoscope is the preferred method if the clinical situation allows. Profound hypotension is usually present, which should be treated immediately with a crystalloid fluid bolus. If hypotension is determined to be due to spinal shock (as opposed to volume depletion from hemorrhage due to other injuries), repetitive fluid boluses are not recommended, and the patient should be started on inotropes to maintain arterial blood pressure. Urinary retention should be assessed, and a urinary catheter should be placed as soon as possible. A thorough neurologic exam utilizing the ASIA score should then be completed. Neurologic examination should also include an assessment of the cranial nerves as they may be independently affected secondary to trauma.
Treatment / Management
Patients with spinal shock will have hypotension and bradycardia due to autonomic dysregulation and imbalance. The sympathetic tone is lost, leading to decreased vascular resistance and hypotension. An unopposed parasympathetic tone leads to bradycardia. Maintaining adequate perfusion pressure to the spine is crucial in patients with spinal shock to prevent secondary ischemic injury. It is generally recommended to maintain mean arterial blood pressure at 85 to 90 mmHg for the first seven days after an acute SCI.
Judicious fluid management is necessary to avoid fluid overload and edema. Most patients will require inotropic therapy. Studies comparing various inotropic therapies in patients with SCI reported improved spinal cord perfusion with norepinephrine and better side-effect tolerance compared with dopamine or phenylephrine. Profound bradycardia can be treated with atropine administration or temporary pacing and is usually seen in patients with higher cervical cord injuries (C1 thru C5). Patients with spinal shock will usually develop paralytic ileus and require decompression. Thermoregulation will also be altered in these patients with spinal shock, requiring external control to maintain body temperature.
Autonomic dysreflexia can also be seen in patients with SCI above the T6 level. Uninhibited sympathetic responses to noxious stimuli below the level of the injury cause vasoconstriction and hypertension in these patients. A compensatory parasympathetic response produces bradycardia and vasodilation above the level of the lesion. This is seen within the first year of injury but is unlikely to occur in the initial time period (first month of injury). Management involves identifying the triggering factor, such as bowel or bladder distention, and treatment with antihypertensive agents.
Orthostatic hypotension due to peripheral vasodilatation is common in the first few months of SCI. Patients with SCI also remain at high risk for pneumonia due to decreased cough reflex and poor secretion clearance. Chest physiotherapy and vaccination should be employed to decrease the risk of this complication. Bowel dysfunction is common after SCI and requires medical therapy to prevent complications. Rectal suppositories are the treatment of choice for managing chronic bowel dysfunction after SCI leading to constipation. Pressure ulcers are also common in patients with SCI and require vigilant pre-emptive skincare. Maintenance of adequate nutritional intake and weight is also crucial in preventing this complication. Pain, depression, and anxiety are common after SCI and should be treated accordingly.
Functional recovery should be the primary goal after the spine has been stabilized. Range-of-motion and resistive exercises, upright positioning, and strengthening exercises should be employed as soon as possible.
Differential Diagnosis
- Cardiogenic shock
- Hypovolemic shock
- Sepsis
- Spinal abscess
- Vertebral fracture
