Neurogenic Shock
Published (updated: ).

Introduction
Neurogenic shock is a devastating consequence of spinal cord injury (SCI). It manifests as hypotension, bradyarrhythmia, and temperature dysregulation due to peripheral vasodilatation following an injury to the spinal cord. This occurs due to the sudden loss of sympathetic tone, with preserved parasympathetic function, leading to autonomic instability. Neurogenic shock is mostly associated with cervical and high thoracic spine injury. Neurogenic shock should be differentiated from hypovolemic shock; the latter is often associated with tachycardia.
Neurogenic shock is not to be confused with a spinal shock which is the flaccidity of muscles and loss of reflexes seen following spinal cord injury.
Early identification and aggressive management are vital in neurogenic shock to prevent secondary spinal injury. This chapter is a concise overview to further aid the care for those patients who develop neurogenic shock.
Etiology
Neurogenic shock is the result of autonomic dysregulation following spinal cord injury, usually secondary to trauma. This dysregulation is due to a loss of sympathetic tone and an unopposed parasympathetic response. A review of the trauma database showed the incidence of neurogenic shock in 19.3% of cervical spine injuries and 7% of thoracic spine injuries. Other causes of neurogenic shock that are far less common include spinal anesthesia, Guillain-Barre syndrome, autonomic nervous system toxins, transverse myelitis, and other neuropathies. The pediatric population reports neurogenic shock in children with trisomy 21, skeletal dysplasia, and tonsillopharyngitis. Neurogenic shock remains a diagnosis of exclusion in a traumatic patient—Advanced Trauma Life Support states that hemorrhagic shock is the more common cause of hypotension. Once that has been managed appropriately, the neurogenic shock should be considered.
Epidemiology
An estimated 8000 to 10,000 people experience traumatic spinal cord injury per year in the United States of America. A review of isolated spinal cord injury from the Trauma Audit and Research Network identified 490 isolated spinal cord injuries. Out of these, the incidence of typical neurogenic shock was only 19.3%. However, a retrospective study at a high volume level 1 trauma center cited as neurogenic shock being present in 19 (31%) of the 62 patients with high cervical spine injuries. There are no defined universal hemodynamic parameters for a neurogenic shock. However, most studies use the definition of systolic blood pressure less than 90 mm Hg and a heart rate of less than 80 bpm. The epidemiology of neurogenic shock is difficult to assess as it is still unknown how hemorrhagic shock and other injuries impact the hemodynamic effects of spinal cord injury.
Pathophysiology
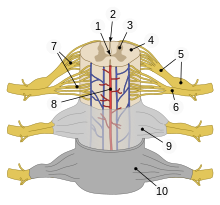
| 1 | central canal |
| 2 | posterior median sulcus |
| 3 | gray matter |
| 4 | white matter |
| 5 | dorsal root & dorsal root ganglion |
| 6 | ventral root |
| 7 | fascicles |
| 8 | anterior spinal artery |
| 9 | arachnoid mater |
| 10 | dura mater |
Neurogenic shock is the clinical state manifested from primary and secondary spinal cord injury. Hemodynamic changes are seen with an injury to the spinal cord above the level of T6. The descending sympathetic tracts are disrupted most commonly from associated fracture or dislocation of vertebrae in the cervical or upper thoracic spine. Primary spinal cord injury occurs within minutes of the initial insult. Primary injury is direct damage to the axons and neural membranes in the intermediolateral nucleus, lateral grey mater, and anterior root that lead to disrupted sympathetic tone. Secondary spinal cord injury occurs hours to days after the initial insult. Secondary injury results from vascular insult, electrolyte shifts, and edema that lead to progressive central hemorrhagic necrosis of grey matter at the injury site. Neurogenic shock is a combination of both primary and secondary injuries that lead to loss of sympathetic tone and thus unopposed parasympathetic response driven by the vagus nerve. Consequently, patients suffer from instability in blood pressure, heart rate, and temperature regulation.
History and Physical
Neurogenic shock can be a difficult diagnosis to make and requires meticulous investigation. Neurogenic shock is most commonly associated with a blunt cervical spine injury. Identification of traumatic cord injury is vital to the investigation of neurogenic shock. Providers should ascertain the mechanism of injury, the presence of midline spinal tenderness, a distracting injury that may take attention from a spinal area, loss of consciousness, neurologic deficits, or intoxication that may misconstrue the exam, as these are associated with a vertebral injury. Though neurogenic shock should be considered only after a hemorrhagic shock has been ruled out in a traumatic patient, the presence of vertebral fracture or dislocation raises the concern for a neurogenic shock. Bradyarrhythmia, hypotension, flushed warm skin are the classic signs associated with neurogenic shock. The joint committee of the American Spinal Injury Association proposed the definition of a neurogenic shock to be general autonomic nervous system dysfunction that also includes symptoms such as orthostatic hypotension, autonomic dysreflexia, temperature dysregulation. A focal neurologic deficit is not necessary for the diagnosis of neurogenic shock.
Evaluation
Before advanced imaging, the neurogenic shock was thought to be associated with spinal cord injury without radiologic abnormality (SCIWORA). With the advent of advanced imaging such as computed tomography (CT) and magnetic resonance imaging (MRI) scans, spinal cord injury is more accurately identified. The diagnosis of neurogenic shock remains a combination of radiographic imaging, hemodynamic monitoring, and clinical exam.
Treatment / Management
Initial management of neurogenic shock is focused on hemodynamic stabilization. Hypotension should be treated first to prevent secondary injury. The first-line treatment for hypotension is intravenous fluid resuscitation. This is to allow appropriate compensation for the vasogenic dilation that occurs. If hypotension persists despite euvolemia, vasopressors and inotropes are the second lines. No single agent is recommended.
Initial c-spine immobilization is important to prevent further spinal cord injury. A cervical collar should be used. Ultimately, surgical intervention may be required for decompression of spinal injury and improvement of neurogenic shock. Symptoms of neurogenic shock have been reported to persist for as long as 4 to 5 weeks.
Differential Diagnosis
- Hypovolemic shock
- Obstructive shock
- Cardiogenic shock
- Septic shock
All these types of shocks are associated with tachycardia, whereas neurogenic shock is associated with bradycardia.
The term “spinal shock” denotes the acute loss of motor, sensory and reflex functions below the level of injury and can be associated with neurogenic shock.
Prognosis
The overall prognosis depends on the extent of spinal cord injury and response to treatment. Those associated with neurological deficits tend to have poor outcomes.
Complications
Complications of neurogenic shock can include severe, protracted hypotension that requires vasopressive therapy and may last as long as 5 weeks post-injury.
