Distributive Shock
Published .
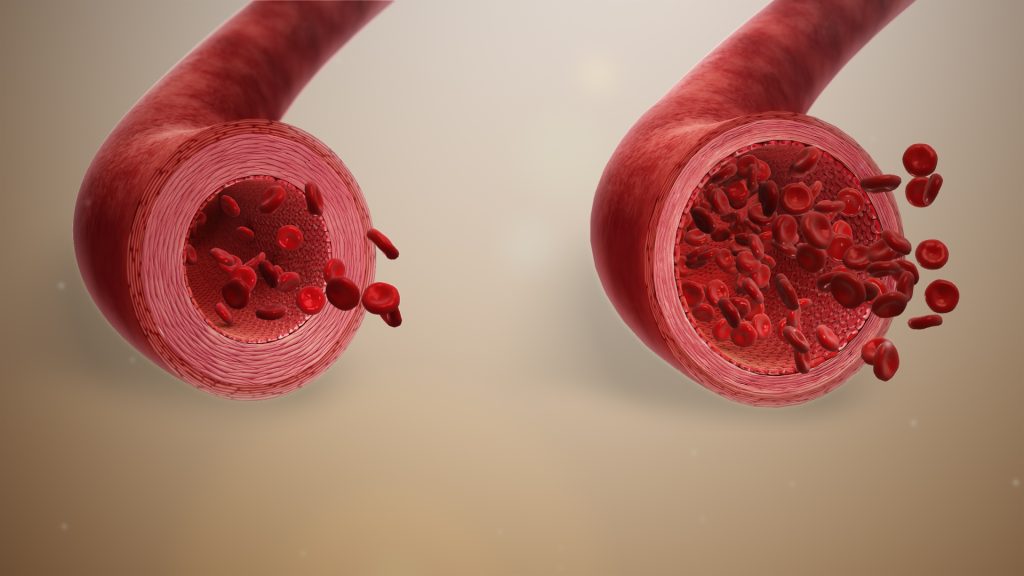
Distributive shock, also known as vasodilatory shock, is one of the four broad classifications of disorders that cause inadequate tissue perfusion. Systemic vasodilation leads to decreased blood flow to the brain, heart, and kidneys causing damage to vital organs. Distributive shock also leads to leakage of fluid from capillaries into the surrounding tissues, further complicating the clinical picture. Due to the complexities of this disease, the causes and treatments for distributive shock are varied.
Etiology
The most common causes of distributive shock in the emergency department are sepsis and anaphylaxis. In cases of trauma, the neurogenic shock should also be on the differential. Other less common causes of distributive shock include adrenal insufficiency and capillary leak syndrome. Drug overdose or toxicity should always be considered, particularly potent vasodilators such as calcium channel blockers and hydralazine.
Distributive shock as a result of sepsis occurs due to a dysregulated immune response to infection that leads to systemic cytokine release and resultant vasodilation and fluid leak from capillaries. These inflammatory cytokines can also cause some cardiac dysfunction, called septic cardiomyopathy, which can contribute to the shock state.
A common cause is the systemic inflammatory response syndrome due to noninfectious causes such as pancreatitis and burns.
In anaphylaxis, the patient typically has a history of previous exposure to an antigen, although this is not required, with resulting IgE formation to that antigen. These IgE molecules then attach to the surface of mast cells in the tissues and basophils in blood. Consequent exposure to the same antigen results in the IgE-mediated release of histamine from mast cells and basophils, leading to systemic vasodilation and capillary fluid leak.
Toxic shock syndrome should be considered in distributive shock. This disease is caused by Staphylococcus aureus and group A streptococci exotoxins that stimulate systemic cytokine release with resulting vasodilation and capillary leak. Historically, this is associated with both vaginal and nasal tampon use.
Neurogenic shock classically occurs in cases of trauma involving the cervical spinal cord. The sympathetic nervous system is damaged resulting in a decreased adrenergic input to the blood vessels and heart, causing vasodilation with resultant hypotension and paradoxical bradycardia.
The distributive shock from adrenal insufficiency occurs due to decreased alpha-1 receptor expression on arterioles secondary to cortisol deficiency, which results in vasodilation. This is seen in patients on chronic steroids that are stopped suddenly.
Capillary leak syndrome, while rare, should be considered in the edematous patient with distributive shock. It occurs due to low blood albumin. Decreased oncotic pressure leads to fluid loss from the blood into the interstitial spaces.
Epidemiology
Septic shock is the most common cause of distributive shock seen in the emergency department. The number of patients admitted with severe sepsis now approaches one million per year with mortality rates extending 50%. It’s crucial to note that nearly 50% of septic patients that present with some degree of end-organ damage will have a cryptic shock, meaning they have inadequate tissue perfusion despite a normal blood pressure reading. Anaphylaxis, likely the second leading etiology of distributive shock, can occur at any age regardless of prior history. Nut allergy and history of asthma have been identified as independent predictors of mortality in patients with anaphylaxis, and great care should be taken when monitoring this subset of patients.
Pathophysiology
In most cases, inflammatory mediators play a major role in the development of distributive shock. Inflammatory cytokines released in both sepsis and toxic shock syndrome induce systemic vasodilation and capillary leak, as well as cardiomyopathy. The systemic release of histamine in anaphylaxis results in similar effects.
Interactions between catecholamines and adrenergic receptors in the blood vessels are crucial in other causes of distributive shock. Both norepinephrine and epinephrine stimulate alpha-1 receptors on arterioles to cause vasoconstriction and regulate blood pressure. In the case of neurogenic shock, the sympathetic nervous system is compromised, leading to reduced catecholamine delivery to these receptors. Cortisol is a key regulator of the expression of alpha-1 receptors on the arteriolar surface, but this becomes compromised in patients with adrenal insufficiency.
In effect, the factors leading to vasodilation and shock are multimodal and complex. This necessitates a careful history and physical examination to elucidate the underlying cause and a multi-system approach to treatment.
History and Physical
If possible, a careful and directed history should be taken directly from the patient. Often this is not possible, and information should be collected from the emergency management service, family members, or other witnesses of the inciting event. Symptoms of infection, like shortness of breath, cough, fever, chills, nausea, vomiting, abdominal pain, and dysuria, as well as an immunocompromised status and recent hospitalizations, should be noted as this information may point to sepsis. Additionally, identifying known allergies and a history of anaphylaxis as well as possible.
Exposures to known allergens can aid the identification of the cause of the patient’s presentation. Review the patient’s medications, particularly steroids and anti-hypertensives, and illicit drug use to determine if overdose or intoxication could be contributing to the clinical picture.
While the physical exam is unreliable in determining the source of shock, some findings can be suggestive of underlying etiology. Warm extremities can point to vasodilation as the cause of shock. A careful skin exam should be completed to identify a cutaneous source of infection such as cellulitis, ulcers, or abscess. Urticaria strongly suggests anaphylaxis.
Always consider adrenal insufficiency in a patient with hypotension, no signs of an infection and showing resistance to usual methods of resuscitation.
The physical exam will reveal:
- Altered mental status
- Tachycardia and tachypnea
- Hypotension
- Warm extremities with bounding pulses in early shock
- Hypo or hyperthermia
- Decreased urine output
- Low oxygen saturation
Evaluation
In undifferentiated patients that present to the emergency department with shock, the exact etiology is often unclear. As always, the evaluation should begin with a primary survey evaluating the airway, breathing, and circulation as well as establishing adequate intravenous (IV) access and hemodynamic monitoring. The patient should be fully exposed and a rapid head to toe examination performed. While definitive airway management is needed in many of these patients, efforts should be made to optimize hemodynamics before intubation to avoid precipitating cardiac arrest. ECG should be obtained rapidly to identify arrhythmias or ischemia which can mimic the clinical picture of distributive shock. Obtain a portable chest x-ray to identify pneumonia, pulmonary edema, or pneumothorax. Bedside ultrasound utilizing the RUSH (Rapid Ultrasound for Shock) exam allows rapid evaluation of global cardiac function and fluid status and helps to identify pericardial tamponade, pulmonary edema, pneumothorax, or occult intra-abdominal hemorrhage. Collect a full spectrum of labs, including lactate, blood and urine cultures, blood gas, and a pregnancy test in females of reproductive age.
Treatment / Management
Regardless of the type of shock, the majority of patients will tolerate and benefit from an initial fluid bolus of 250-500 mL. Patients with distributive shock are significantly more likely to require vasopressor support. The ultimate goal is to achieve adequate tissue perfusion utilizing fluid resuscitation and vasopressors.
For cases of anaphylactic shock, epinephrine is the pressor of choice, as it offers alpha-1 and beta-1 stimulation similar to norepinephrine but also provides beta-2 stimulation, which stimulates bronchodilation and stabilization of mast cells and basophils. Adjunct interventions will include both H1 and H2 antihistamines, steroids, albuterol, fluids, and potentially glucagon for those using beta-blockers.
The shock that is unresponsive to both fluids and vasopressors may indicate adrenal insufficiency. In such cases, steroids can be given to the increased arteriolar expression of alpha-1 receptors. Hydrocortisone 100 mg is the typical treatment.
In cases where vasopressor drips are not immediately available, and the patient has critically low perfusion pressure (particularly MAP less than 50 mmHg, the critical perfusion pressure to the brain), push dose vasopressors can be utilized. Epinephrine and phenylephrine are common agents of choice for this purpose.
Soon after resuscitation consider a diet. Some patients may require tube feedings and others may require parenteral feeding.
Differential Diagnosis
- Anaphylaxis
- CO poisoning
- Adverse drug reaction
- Neurogenic shock
- Toxic shock syndrome
- Cyanide poisoning
- Cardiogenic shock
- Hemorrhagic shock
- Tamponade
Prognosis
The mortality from distributive shock varies on the cause and can range from 20-80%. Early recognition is the key to improved survival. Higher mortality rates are linked to:
- Positive blood cultures
- Advanced age
- Elevated serum lactate or failure to clear lactate when labs are repeated
- Infection due to pseudomonas aeruginosa
- Alcohol use
- Immunocompromised state
- Poor functional status prior to the event
