Angina vs Acute Coronary Syndrome
Published .
Angina
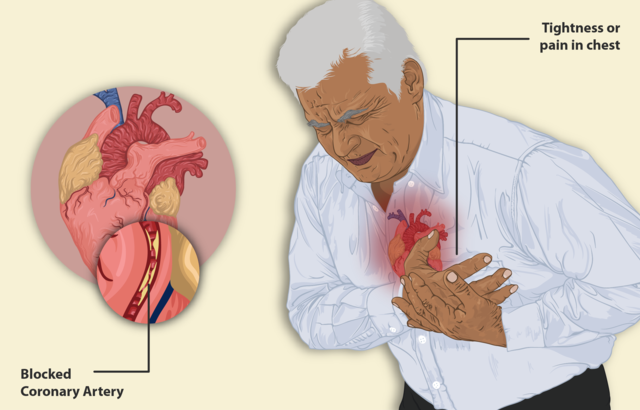
Angina is chest pain or discomfort you feel when there is not enough blood flow to your heart muscle. Your heart muscle needs the oxygen that the blood carries. Angina may feel like pressure or a squeezing pain in your chest. It may feel like indigestion. You may also feel pain in your shoulders, arms, neck, jaw, or back.
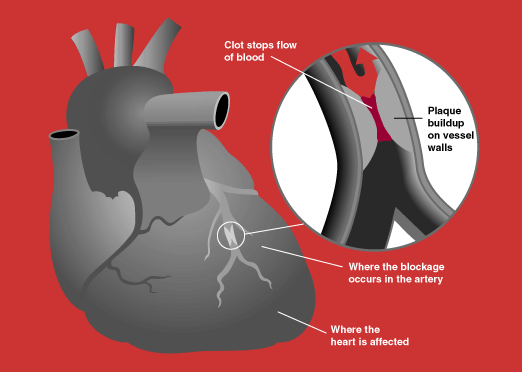
Angina is a symptom of coronary artery disease (CAD), the most common heart disease. CAD happens when a sticky substance called plaque builds up in the arteries that supply blood to the heart, reducing blood flow.
There are three types of angina:
- Stable angina is the most common type. It happens when the heart is working harder than usual. Stable angina has a regular pattern. Rest and medicines usually help.
- Unstable angina is the most dangerous. It does not follow a pattern and can happen without physical exertion. It does not go away with rest or medicine. It is a sign that you could have a heart attack soon.
- Variant angina is rare. It happens when you are resting. Medicines can help.
Acute Coronary Syndrome
Introduction
Acute coronary syndrome (ACS) refers to a group of conditions that include ST-elevation myocardial infarction (STEMI), non-ST elevation myocardial infarction (NSTEMI), and unstable angina. It is a type of coronary heart disease (CHD), which is responsible for one-third of total deaths in people older than 35. Some forms of CHD can be asymptomatic, but ACS is always symptomatic.
Etiology
ACS is a manifestation of CHD (coronary heart disease) and usually a result of plaque disruption in coronary arteries (atherosclerosis). The common risk factors for the disease are smoking, hypertension, diabetes, hyperlipidemia, male sex, physical inactivity, family obesity, and poor nutritional practices. Cocaine abuse can also lead to vasospasm. A family history of early myocardial infarction (55 years of age) is also a high-risk factor.
Epidemiology
CHD affects about 15.5 million in the United States. The American Heart Association estimates a person has a heart attack every 41 seconds. Heart disease is the leading cause of death in the United States. Chest pain is among the top reasons for emergency department visits.
Pathophysiology
The underlying pathophysiology in ACS is decreased blood flow to part of heart musculature which is usually secondary to plaque rupture and formation of thrombus. Sometimes ACS can be secondary to vasospasm with or without underlying atherosclerosis. The result is decreased blood flow to a part of heart musculature resulting first in ischemia and then infarction of that part of the heart.
History and Physical
The classic symptom of ACS is substernal chest pain, often described as crushing or pressure-like feeling, radiating to the jaw and/or left arm. This classic presentation is not seen always, and the presenting complaint can be very vague and subtle with chief complaints often being difficulty breathing, lightheadedness, isolated jaw or left arm pain, nausea, epigastric pain, diaphoresis, and weakness. Female gender, patients with diabetes, and older age are all associated with ACS presenting with vague symptoms. A high degree of suspicion is warranted in such cases.
In the physical exam, general distress and diaphoresis are often seen. Heart sounds are frequently normal. At times, gallop and murmur can be heard. Lung exam is normal, although at times crackles may be heard pointing toward associated congestive heart failure (CHF). Bilateral leg edema may be present indicating CHF. The rest of the systems are typically within normal limits unless co-pathologies are present. The presence of abdominal tenderness to palpation should make the provider consider other pathologies like pancreatitis and gastritis. The presence of unequal pulses warrants consideration of aortic dissection. The presence of unilateral leg swelling should warrant work-up for pulmonary emboli. Hence a thorough physical exam is very important to rule out other life-threatening differentials.
Evaluation
The first step of evaluation is an ECG, which helps differentiate between STEMI, NSTEMI, and unstable angina. American Heart Association guidelines maintain that any patient with complaints suspicious of ACS should get an ECG within 10 minutes of arrival. Cath lab should be activated as soon as STEMI is confirmed in a percutaneous coronary intervention (PCI) center. Cardiac enzymes especially troponin, CK-MB/CK ratio is important in assessing the NSTEMI versus myocardial ischemia without tissue destruction. A chest x-ray is useful in diagnosing causes other than MI presenting with chest pain like pneumonia and pneumothorax. The same applies for blood work like complete blood count (CBC), chemistry, liver function test, and lipase which can help differentiate intraabdominal pathology presenting with chest pain. Aortic dissection and pulmonary emboli should be kept in differential and investigated when the situation warrants.
