PETCo2 = Capnometry
Published (updated: ).
Capnometry is a non‐invasive monitoring technique which allows fast and reliable insight into ventilation, circulation, and metabolism. In the prehospital setting it is mainly used to confirm correct tracheal tube placement. In addition it is a useful indicator of efficient ongoing cardiopulmonary resuscitation due to its correlation with cardiac output, and successful resuscitation. It helps to confirm the diagnosis of pulmonary thromboembolism and to sustain adequate ventilation in mechanically ventilated patients. In patients with hemorrhage, capnometry provides improved continuous hemodynamic monitoring, insight into adequacy of tissue perfusion, optimization within current hypotensive fluid resuscitation strategy, and prevention of shock progression through controlled fluid administration.
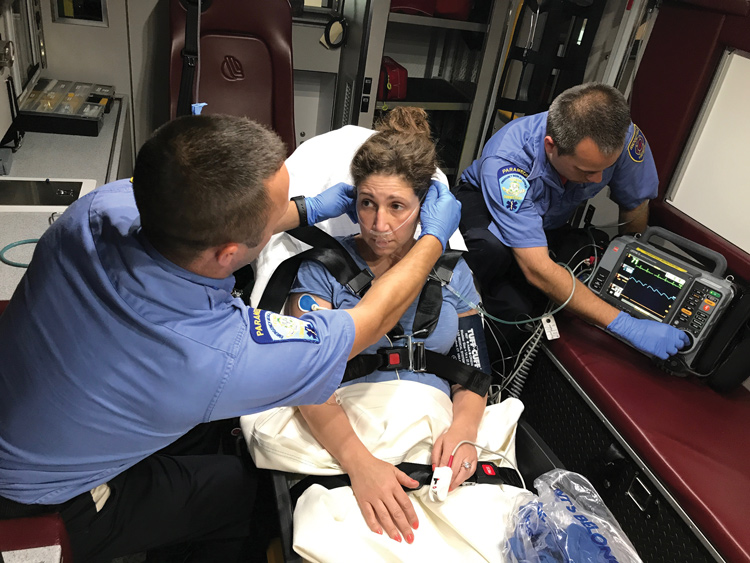
Managing the critically ill patient is one of the most challenging aspects of prehospital emergency care. The nature of work in such circumstances demands methods which rapidly recognize patients at risk. Capnometry, as a non‐invasive method, offers fast and reliable insight into certain pathophysiological processes and aids in the clinical evaluation of critically ill patients, especially those in cardiac arrest and requiring cardiopulmonary resuscitation, and assists in the monitoring patients after endotracheal intubation and mechanical ventilation.
For many years aggressive fluid resuscitation has been a mainstay in the early treatment of the patient in hemorrhagic shock. But in recent years hypotensive fluid resuscitation before surgical repair of uncontrolled thoraco‐abdominal hemorrhage has proven to be superior over aggressive fluid resuscitation. Methods like capnometry could allow better additional discrimination between therapeutic demands, leading to more precise fluid resuscitation in the prehospital setting. In fact, changes in end tidal carbon dioxide partial pressure (Petco2) promptly reflect circulatory compromise and as such help in timely recognition of patients at risk.
Basic physiology of carbon dioxide and end tidal carbon dioxide measurements

Carbon dioxide (CO2) is the product of cellular aerobic metabolism. It diffuses easily from cells into blood and erythrocytes and is transported to the lungs by venous blood through the function of cardiac output. Under normal conditions of circulation and ventilation the partial pressure of CO2 approaches 50 mm Hg at the level of tissues, and 45 mm Hg in the venous blood. The difference between the latter and alveolar CO2 partial pressure (Paco2) which is around 40 mm Hg, is responsible for diffusion of CO2 into the alveoli. There, CO2 is eliminated from the body with minute ventilation. Arterial CO2 partial pressure (Paco2) normally varies from 35–45 mm Hg.
Approximately 7% of CO2 is dissolved in blood. The rest of it diffuses into erythrocytes where 23% of CO2 reversely bonds to hemoglobin, and the rest forms carbonic acid with water after carbonic anhydrase mediated enzymatic reaction. Carbonic acid dissolves into hydrogen and bicarbonate ion. The former is buffered by deoxygenated hemoglobin in tissues, and the latter can be exchanged with plasma chloride ions. In lung capillaries these reactions are reversed: bicarbonate enters erythrocytes, binds to hydrogen ions recently released from oxygenated hemoglobin, and dissolves into CO2 and water.
Capnometry in monitoring and diagnostics
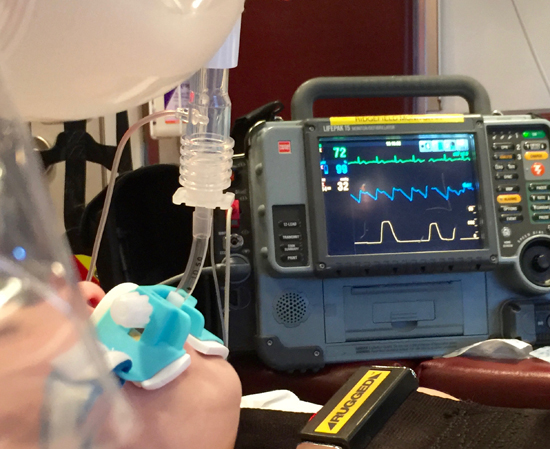
Confirmation of correct endotracheal tube placement is of paramount importance because esophageal intubation increases morbidity and mortality if unrecognized. Capnometry, and capnography with typical waveform in particular, are the most reliable methods to confirm tracheal intubation.
In cardiac arrest Petco2 values decrease abruptly almost to zero. They increase with the start of chest compressions during CPR, and as spontaneous circulation resumes they return to normal or above normal levels. As the cardiac arrest occurs, cardiac output no longer serves as a conduit between the large peripheral tissue compartment where production of CO2 is generated, and the smaller central pulmonary compartment where elimination of CO2 takes place. The result is accumulation of CO2 in the tissues and a drastic fall in alveolar and consequently end tidal CO2. Therefore initial values of Petco2 after endotracheal intubation and resumed ventilation are low. Initiation of chest compressions restores a fraction of normal cardiac output and begins to wash CO2 out of the peripheral tissue compartment, where CO2 is now produced in part by aerobic metabolism and in part by anaerobic metabolism. The latter is caused by buffering of metabolic acids by bicarbonate, which leads to carbonic acid production and its dissociation to CO2 and water.
What can you figure out with Petco2?
Return of Spontaneous Circulation
Establishing cardiac output with CPR re‐establishes CO2 transport and causes alveolar CO2 tension to increase which ultimately results in increased Petco2 values. But cardiac output produced by closed chest compressions is only a fraction of normal cardiac output, so the Petco2 values are usually lower than normal. Return of spontaneous circulation is usually indicated by a rapid increase in Petco2 since normal or near‐normal cardiac output increases alveolar and therefore end tidal CO2 partial pressure. However, initial and final values of Petco2 of ⩽10 mm Hg during CPR proved to predict mortality, which makes capnometry also an important tool in the prognostication of cardiac resuscitation. Capnometry in CPR thus provides information about efficacy of chest compressions, return of spontaneous circulation, and prognosis of outcome after cardiac arrest.
Capnometry can also help to differentiate an asphyxic from primary cardiac arrest, detect waning neuromuscular blockade, and serves as an additional diagnostic tool in pulmonary thromboembolism. In patients with asphyxia as the cause of cardiac arrest, initial Petco2 values after endotracheal intubation are much higher than in patients with primary cardiac arrest due to ventricular fibrillation and/or ventricular tachycardia. Asphyxial cardiac arrest leads to continued cellular production of CO2 and continued cardiac output before cardiac arrest that allows delivery of CO2 to the lungs which ultimately increases alveolar CO2. This in turn is reflected as high Petco2 once ventilation is resumed during CPR. However, the difference in Petco2 between primary and secondary cardiac arrest is no longer present after 1 min of CPR. The initial Petco2 difference thus serves as a good diagnostic tool for reassuring emergency physicians to take measures appropriate for asphyxial cardiac arrest, since the hypoxia is a potentially reversible cause of cardiac arrest.
In pulmonary thromboembolism Petco2 values are characteristically lower than normal because of diminished pulmonary perfusion and increased alveolar dead space, and consequently decreased CO2 elimination capability. Retention of CO2 leads to increased venous carbon dioxide partial pressure (Pvco2) and Paco2, which ultimately increases arterial to end tidal CO2 gradient. This helps further in reaching a correct diagnosis, especially in silent pulmonary embolism.
In hemorrhage, changes in Petco2 reflect hemodynamic changes. This allows not only prompt recognition of circulatory compromise but also more precise fluid resuscitation. Capnometry is the only continuous non‐invasive monitoring method in the prehospital setting which gives indirect information about tissue perfusion through its correlation with oxygen supply dependency during hemorrhagic shock. It is also of value in predicting outcome from major trauma and trauma surgery where P(a–et)co2 difference >10 mm Hg can predict mortality even if blood pressure is normalised.
Petco2 values can be measured in intubated and non‐intubated patients, even though hyperventilation can alter measurements. The latter is successfully achieved with a nasal cannula, especially in children. Measurements taken through a facial mask are less accurate compared to a nasal cannula because of increased dead space, which decreases the amount of CO2 in expired air. Oxygen supplementation can affect measurements of Petco2, but not significantly.
However, there are some limitations in the interpretation of Paco2 on the basis of Petco2 measurements in critically ill patients. In any cardiorespiratory dysfunction, including breathing patterns which cause incomplete alveolar emptying, and some pharmacological interventions which are used in treating low flow states, P(a–a)co2 and consequently P(a–et)co2 difference increases due to ventilation–perfusion mismatch. These limitations do not support Petco2 measurements as a substitute for Paco2 measurements.
Nevertheless, in the prehospital setting it is sudden changes of Petco2 that make capnometry an important tool for early detection of mainly circulatory and/or ventilatory compromise in the critically ill, and not the relationship between Petco2 and Paco2. A sudden decrease in Petco2 is caused by sudden hypotension, sudden hyperventilation, massive pulmonary embolism, occlusion of the endotracheal tube, and disconnection or leakage in the artificial ventilatory system, while decreased CO2 production and hyperventilation cause a more gradual decline in Petco2. A sudden increase in Petco2 is caused by a sudden increase in cardiac output, such as when spontaneous circulation returns after CPR, and following an injection of sodium bicarbonate, while hypoventilation and increased CO2 production cause more gradual increases in CO2. Therefore, a final interpretation of Petco2 must be made after all parameters which affect measurements have been accounted for—that is, ventilation and circulatory parameters, metabolism, and technical errors.
Sublingual capnometry shows great promise for the early recognition of patients at risk of tissue hypoperfusion, hypoxia, and shock progression, because it avoids disturbances of measurements caused by hyperventilation.
Petco2 as an indicator of hemorrhage and tissue perfusion adequacy
In uncontrolled hemorrhage, cardiac output and blood pressure decrease. In early stages of hemorrhage, cardiac output decreases before changes in blood pressure can be detected. The relationship between cardiac output and Petco2, even in low flow states, makes Petco2 an indicator of changes in cardiac output. Hemodynamic changes lead to immediate changes in Petco2; this makes Petco2 a good indicator of an early stage hemorrhage due to early detection of changes in cardiac output.
According to Fick’s principle, cardiac output equals the relationship between oxygen consumption and arteriovenous difference in oxygen concentration. Decreased cardiac output leads to decreased tissue oxygen consumption. Under physiological conditions oxygen consumption is constant because oxygen supply is greater than its consumption. A critical decrease in oxygen supply makes oxygen consumption supply‐dependent. This marks the initiation of anaerobic metabolism. Increased lactate, hypercapnia in gastric mucosa blood vessels, and increased arteriovenous difference in CO2 partial pressure all indicate tissue hypoperfusion and hypoxia at this point. Constant minute ventilation, changes in Petco2 correlate well with changes in oxygen consumption in hemorrhagic shock, and these changes also indicate the onset of oxygen supply dependency during hemorrhagic shock. Fluid resuscitation increases oxygen consumption due to its increased delivery, which ultimately increases Petco2.
Capnometry guided fluid resuscitation in uncontrolled internal hemorrhage

The strategy of fluid resuscitation in hypovolemic shock caused by hemorrhage has been thoroughly debated in recent years. Aggressive fluid resuscitation dilutes clot factors, dislodges formed blood clots, and leads to further bleeding, especially in parenchymal organ trauma. These factors are associated with increased blood loss and mortality, so that aggressive fluid therapy may be harmful to patients with uncontrolled thoraco‐abdominal hemorrhage. However, aggressive fluid resuscitation is still considered appropriate in controllable hemorrhage (head and isolated extremity trauma) and in trauma patients without a palpable pulse. In patients with uncontrolled thoraco‐abdominal hemorrhage, limited or hypotensive fluid resuscitation avoids detrimental effects of an early aggressive resuscitation, decreases mortality, and is currently considered more appropriate for short periods before surgical repair, even at the expense of tissue perfusion.
Nevertheless, at an early stage of hemorrhage blood pressure can still be normal, even with substantial blood loss, and significant delay in fluid resuscitation, based on clinical signs and normal blood pressure measurement alone, can be detrimental because of decreased tissue perfusion and shock progression. Changes in Petco2 are an immediate reaction to hemorrhage, and any decrease in cardiac output would cause Petco2 to decrease, indicating hemorrhage in progress. It is an intriguing thought that capnometry guided fluid resuscitation could avoid delay in initiating fluid resuscitation due to prompt detection of these hemodynamic changes. It could also help to enhance tissue perfusion by adjusting further fluid administration, while keeping the blood pressure in appropriate ranges at the same time. This could significantly improve not only the clinical evaluation but also the fluid administration strategy in patients with uncontrolled hemorrhage.
On the other hand, there is also a possibility of severe under‐resuscitation as a potential complication of hypotensive fluid resuscitation strategy in hemorrhagic shock. Capnometry could prevent this complication through prompt detection of a decrease in Petco2. In order to maintain normal or near normal Petco2 values, and tissue perfusion as well, increased amounts of infused fluids help to overcome this problem. More research is needed to confirm the usefulness of capnometry in decision making in patients with uncontrolled internal hemorrhage.
Conclusion
In the prehospital setting capnometry is an important tool in the diagnosis, monitoring, and prediction of outcome. Even though there are some limitations of Petco2 monitoring in critically ill patients, sudden changes in Petco2 promptly reflect circulatory and/or ventilatory compromise. Prompt reaction to acute hemodynamic changes in patients with constant minute ventilation, together with other measures of clinical evaluation, helps in timely detection of patients at risk in the prehospital setting. For that reason capnometry, especially sublingual, can also be an important non‐invasive monitoring method in patients with uncontrolled internal hemorrhage in the prehospital setting, together with the control of fluid resuscitation through indirect control over tissue perfusion, especially in limited fluid resuscitation. This could ultimately help to impede shock progression and further bleeding at the same time.
