Complications of Mechanical Ventilation
Published (updated: ).
Introduction

Barotrauma is damage to body tissue secondary to pressure difference in enclosed cavities within the body. Barotrauma is commonly observed in scuba divers, free-divers, or even in airplane passengers during ascent and descent. The most common organs affected by barotrauma are the middle ear (otic barotrauma), sinuses (sinus barotrauma), and the lungs (pulmonary barotrauma).
Pulmonary barotrauma is a complication of mechanical ventilation and has correlations with increased morbidity and mortality. The natural mechanism of breathing in humans depends on negative intrathoracic pressures. In contrast, patients on mechanical ventilation ventilate with positive pressures. Since positive pressure ventilation is not physiological, it may lead to complications such as barotrauma. Pulmonary barotrauma is the presence of extra alveolar air in locations where it is not present under normal circumstance. Barotrauma is most commonly due to alveolar rupture, which leads to an accumulation of air in extra alveolar locations. Excess alveolar air could then result in complications such as pneumothorax, pneumomediastinum, and subcutaneous emphysema. Mechanical ventilation modalities include invasive mechanical ventilation and non-invasive mechanical ventilation, such as bilevel positive airway pressure. The incidence of barotrauma in patients receiving non-invasive mechanical ventilation is much lower when compared to patients receiving invasive mechanical ventilation. Patients at high risk of developing barotrauma from mechanical ventilation include individuals with predisposing lung pathology such as chronic obstructive pulmonary disease (COPD), asthma, interstitial lung disease (ILD), pneumocystis jiroveci pneumonia, and acute respiratory distress syndrome (ARDS).
Etiology
Pulmonary barotrauma results from positive pressure mechanical ventilation. Positive pressure ventilation may lead to elevation of the trans-alveolar pressure or the difference in pressure between the alveolar pressure and the pressure in the interstitial space. Elevation in the trans-alveolar pressure may lead to alveolar rupture, which results in leakage of air into the extra-alveolar tissue.
Every patient on positive pressure ventilation is at risk of developing pulmonary barotrauma. However, certain ventilator settings, as well as specific disease processes, may increase the risk of barotrauma significantly. When managing a ventilator, physicians and other health care professionals must be aware of these risks to avoid barotrauma.
Specific disease processes, including chronic obstructive pulmonary disease (COPD), asthma, interstitial lung disease (ILD), pneumocystis pneumonia, and acute respiratory distress syndrome (ARDS), may predispose individuals to pulmonary barotrauma. These diseases are associated with either dynamic hyperinflation or poor lung compliance, both of which predispose patients to increased alveolar pressure and ultimately barotrauma.
Patients with obstructive lung disease, COPD, and asthma are at risk of dynamic hyperinflation. These patients have a prolonged expiratory phase, and therefore have difficulty exhaling the full volume before the ventilator delivers the next breath. As a result, there is an increase in the intrinsic positive end-expiratory pressure (PEEP), also known as auto-PEEP. The hyperinflation is progressive and worsens with each tidal volume delivered. It leads to overdistention of the alveoli and increases the risk for barotrauma. Dynamic hyperinflation can be managed by decreasing the respiratory rate, decreasing the tidal volume, prolonging the expiratory time, and in some cases by increasing the external PEEP on the ventilator.
Pathophysiology
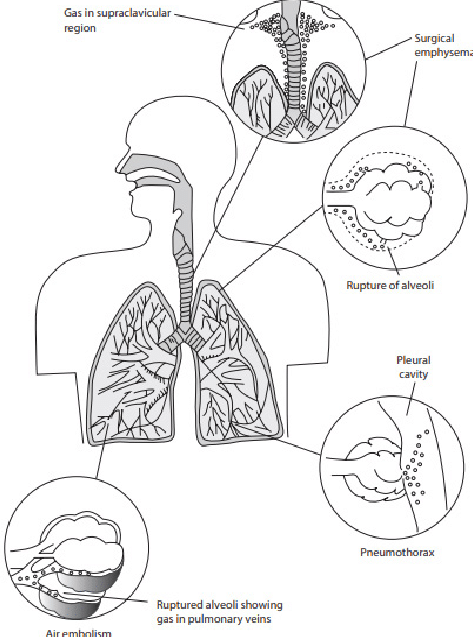
The exact pathophysiology for lung injury and barotrauma due to mechanical ventilation remains unclear; however, evidence suggests that overdistention and increased pressures in the alveoli units lead to inflammatory changes and possibly rupture and leakage of air into the extra alveolar tissue.
Researchers have described several mechanisms in the literature for the rupture of alveoli. Most of the mechanisms have their basis in overdistention and increased pressures in the alveoli. Historically, large tidal volumes were the approach in patients requiring mechanical ventilation to minimize atelectasis and improve oxygenation and ventilation. Such ventilatory settings usually lead to high inspiratory pressures and overdistention of the alveolar unit. Overdistention is more pronounced in patients with ARDS and other non-uniform lung diseases. In non-uniform lung disease, not every alveoli unit is affected equally; normal alveoli receive a greater percentage of the tidal volume, which leads to preferential ventilation and ultimately overdistention to accommodate the larger tidal volume.
History and Physical
The history and physical exam in patients with barotrauma secondary to mechanical ventilation are usually limited since those patients are sick and under sedation while on mechanical ventilation. In cases of clinically significant pneumothorax, patients will present with acute changes in vital signs, including tachypnea, hypoxia, and tachycardia. Patients may also present with obstructive shock if a tension pneumothorax occurs. Physical examination may be significant for absent breath sounds if a pneumothorax exists. Subcutaneous emphysema may also present in some cases. In some, less severe cases, no systemic or hemodynamic changes may be present.
Differential Diagnosis
- Acute respiratory distress syndrome (ARDS)
- Bacterial/viral pneumonia
- Aspiration pneumonitis
- Shock (distributive, cardiogenic, hemorrhagic)
- Flail chest, chest trauma
- Secondary pneumothorax
- Pulmonary emboli
- Asthma exacerbation
- COPD exacerbation
- Acute coronary syndrome
Complications
Patients who develop barotrauma secondary to mechanical ventilation also end up staying in the ICU and on mechanical ventilation for a more extended period. Prolonged time on mechanical ventilation may result in further complications secondary to barotrauma as well as others, including ventilator-associated pneumonia, delirium, intensive care acquired weakness, and nosocomial infections.
