Artificial Ventilation
Published (updated: ).
Introduction
Positive pressure ventilation is a form of respiratory therapy that involves the delivery of air or a mixture of oxygen combined with other gases by positive pressure into the lungs. As gas enters the lungs, the interalveolar pressure increases until a change in flow or pressure are detected by the machine delivering the mixture, or the set volume of gas was delivered to signal the end of a breath. Expiration of air happens passively secondary to the build-up of pressure in the alveoli that escapes into the less pressurized conductive airways. Historically, artificial lung ventilation based on the opposite to PPV physical principle – the negative pressure ventilation – was used widely to treat acute respiratory failure in poliomyelitis patients via hermetically sealing the patient’s torso inside the vacuum-producing “iron lung” machine. The overwhelming polio epidemic of Copenhagen in 1952 and insufficient availability of “iron lungs” led to the implementation of PPV into clinical practice.
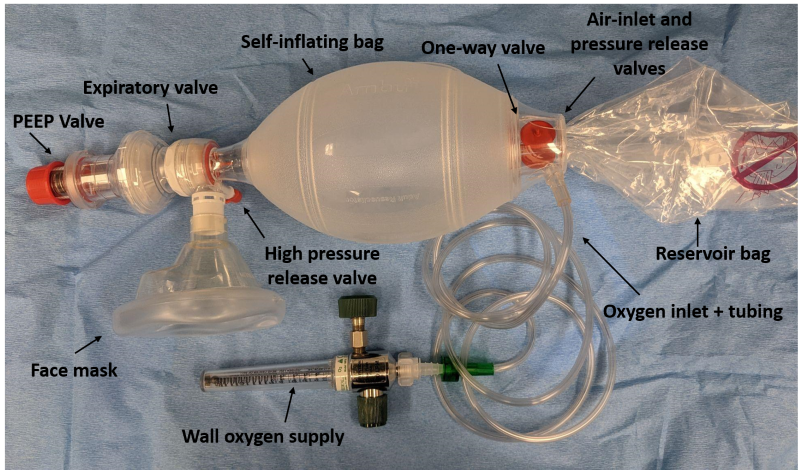
Positive pressure ventilation can be delivered in two forms: non-invasive positive pressure ventilation (NIPPV), which is delivered through a special face mask with a tight seal (air travels through anatomical airways), or invasive positive pressure ventilation (IPPV), which involves the delivery of positive pressure to the lungs through an endotracheal tube or tracheostomy (or any other device that delivers gas bypassing parts of the anatomical airway). Each form of ventilation has its own benefits, risks, indications, and contraindications.
Anatomy and Physiology
A basic understanding of the anatomy of the upper and lower airway is essential to comprehend respiratory physiology and the interplay between inspiratory and expiratory forces that work together to form a breath. The upper airway is the first part of the respiratory system that has an important role in conducting air towards the lungs. It begins with the nasal cavity and continues onto the nasopharynx and oropharynx, down to the larynx and trachea. The mucosa, cartilages, neural, and lymphatic system of upper airways affect the flow and physical qualities of the air that is inhaled. Likewise, they have an impact on the delivery of positive pressure ventilation. It may be difficult to administer PPV via mask ventilation in patients with congenital facial defects, defects secondary to trauma, or in obese patients with excess soft tissue who often suffer from obstructive sleep apnea (OSA).
The lower airway continues down below the vocal folds to the trachea to form the right and left mainstem bronchi, which further divide into smaller segmental bronchi. These subdivide into even smaller bronchioles that eventually end with the terminal portion of the airway, the alveoli, in which gas exchange occurs.
When endotracheal intubation is performed, the tube is positioned in the trachea with the cuff inflated below the vocal cords. In the most technical sense, a breath during PPV can be characterized by changes in pressure, volume, and flow during inspiration and expiration.
Indications
The indications to initiate positive pressure ventilation and more specifically, mechanical ventilation, are many, some of the major indications include:
- Airway protection in a patient who cannot maintain or protect an open airway, e.g., from an altered level of consciousness or trauma
- Hypercapnic respiratory failure
- Hypoxemic respiratory failure
- Circulatory failure

Personnel
The application of positive pressure ventilation, and more specifically, mechanical ventilation requires a trained group of healthcare providers open to communication that have a fundamental understanding of ventilators and positive pressure devices.
Complications
The complications associated with positive pressure ventilation are many and can be quite serious. This is why a thorough understanding of its use is required by an interprofessional group of medical providers. Most complications will focus specifically on classic mechanical ventilation as its exact nature is more invasive, and it is important to understand its consequences. However, although rarer, complications can and do occur, with non-invasive positive pressure ventilation.
Ventilator-associated Lung Injury and Barotrauma
Barotrauma occurs when there is alveolar damage due to high pressures entering the lungs. Specifically, the transalveolar pressure, which is the difference in pressure between the alveolus and the surrounding interstitial space, is increased to such an extent that the epithelial lining of the alveoli is damaged. With repeated breaths and inappropriate ventilation, the damage often occurs on a microscopic level until it is severe enough to cause an overt pneumothorax, subcutaneous emphysema, or pneumomediastinum, which are all conditions associated with high mortality rates.
Excessively high tidal volumes or inspiratory pressures are some of the underlying culprits in the cause of barotrauma. One of the landmark studies on acute respiratory distress syndrome, known as ARDS demonstrated that using lung-protective strategies with lower tidal volumes (between 4-8 mL/kg based on ideal body weight) have improved mortality benefits and are associated with more ventilator-free days for patients. Additional studies have examined lung protective strategies for patients not suffering from acute lung injury and have also found reduced morbidity and mortality benefits, although additional studies are needed for conclusive evidence.
Hemodynamic Effects
Positive pressure ventilation results in physiologic alterations in intrathoracic pressure and cardiac output. One of the most common hemodynamic effects from positive pressure ventilation is a reduction in preload to the heart secondary to increased intrathoracic pressure that obstructs blood flow to the inferior vena cava and right atrium. This effect is more prominent in individuals that may already have reductions in intravascular volume. Likewise, changes in intrathoracic pressure or cardiac output can precipitate an arrhythmia or myocardial ischemia.
Even though most arrhythmias are related to structural changes in the heart, it is common for them to occur secondary to positive pressure ventilation. This is because ventilated patients often have respiratory and electrolyte derangements, including hypoxemia, hypercapnia, acidemia, alkalemia, hypokalemia, hypomagnesemia, or hypocalcemia. Serial arterial blood gasses are often obtained to identify and correct underlying derangements and prevent arrhythmias. Likewise, mechanical ventilation and critical illness lead to hormonal and catecholamine changes in the body that can precipitate myocardial ischemia. This process can occur at any time while a patient requires mechanical ventilation but is also likely during weaning trials when myocardial oxygen demand is increased, and a patient’s sedation is decreased or turned off to assess their ability to come off the ventilator.
Ventilator-associated Pneumonia
The most common infection among mechanically ventilated patients receiving positive pressure ventilation is ventilator-associated pneumonia (VAP). The mortality rate is high and can range between 20% to 50%. An endotracheal tube serves the purpose of protecting a patient’s airway from aspiration and providing a path for the flow of air between the patient and the ventilator. However, it also serves as a conduit between the world and the normally sterile lower respiratory tract. In the setting of critical illness and reduced immune system function, bacteria often invade and colonize the lower respiratory tract of patients causing VAP.
Critically ill patients that require positive pressure ventilation or mechanical ventilation are often hypoxemic and require high levels of inspired oxygen (FIO2). However, not all conditions that require a patient to be mechanically ventilated require high levels of oxygen therapy. In fact, high levels of oxygen can be toxic to the human body. Areas of the lungs with ventilation-perfusion mismatches under high FIO2 can actually lead to a phenomenon known as re-absorption atelectasis that will further aggravate any ventilation-perfusion mismatches. High oxygen levels are also associated with increased vasoconstrictive effects on coronary circulation and increased mortality from cardiac causes.
Neuromuscular Complications
Patients that require mechanical ventilation often need sedation due to the stimulating nature of the endotracheal tube. Likewise, the act of being on a ventilator can be a traumatic experience. Some patients that are in desynchrony with the ventilator, colloquially known as “fighting the vent,” may require paralytic medications such as rocuronium so that they can be safely ventilated to treat their underlying condition. However, important neurochemical changes occur within patients’ bodies, such as the depletion of bioenergetic neuron reserves, altered sodium channel activation, and increased inflammatory cytokines, which lead to changes such as atrophy of the diaphragm or critical illness myopathy.
These changes make it difficult to wean patients off the ventilator and may require the patient to undergo a separate surgical procedure known as a tracheostomy to create an opening in the neck to place a tracheostomy tube for further ventilatory support based on the patient’s underlying critical illness. These patients often require prolonged mechanical ventilation.
Clinical Significance

Modern medicine has made significant strides in the treatment of complex cardiovascular and respiratory illnesses. With the advent of ventilators in the past century, and their continued development and improvement, remarkable progress has been made in treating patients that normally would have succumbed to their illness.
Some disease processes would most certainly lead to death if it were not for the ability to ventilate and oxygenate a patient. However, the therapeutic window for providing positive pressure ventilation is very narrow, and a thorough understanding is required of its use in order to garner its benefits.
