Airway Management
Published (updated: ).
Introduction
To be skillful at airway management, the provider must know the critical anatomical, physiological, and pathological features related to the airway. They should also be aware of the various tools and methods that have been developed for this purpose. It is additionally important to know the indications, contraindications, and complications of endotracheal intubation. It is vital to understand how to assess the confirmation of the placement of an advanced airway. Additionally, knowing the differences between the adult, pediatric, and neonatal airways and being well versed with difficult airways is vital as these can significantly impact safe and effective airway control.
The four principals of airway management in Advanced Cardiovascular Life Support are:
- Is the airway patent?
- Is the advanced airway indicated?
- Is the proper placement of the airway device confirmed?
- Is the tube secure, and is the placement of the tube confirmed frequently?
Indications
Indications for intubation to secure the airway include respiratory failure (hypoxic or hypercapnic), apnea, a reduced level of consciousness (sometimes stated as GCS less than or equal to 8), rapid change of mental status, airway injury or impending airway compromise, high risk for aspiration, or ‘trauma to the box (larynx),’ which includes all penetrating injuries to the neck, abdomen, or chest.
Equipment
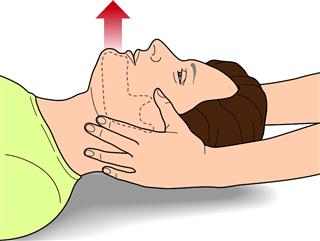
Airway Position and Clearance
Upper airway obstruction can be relieved by head tilt, chin lift, or jaw thrust. In infants and children, a simple suctioning of the airway will help with the clearance. The bulb syringe or any other mechanical suction device can clear mucus or other debris from the airway. When using a bulb syringe to suction an infant, it is important to suction the mouth before the nose to avoid aspiration. The first step is to depress the bulb syringe and then place it in the mouth, then the nose. Infants are prone to vagal stimulation, and suctioning can lead to bradycardia. Suction must not last for over 10 seconds.
Adjuncts to Upper Airway Obstruction
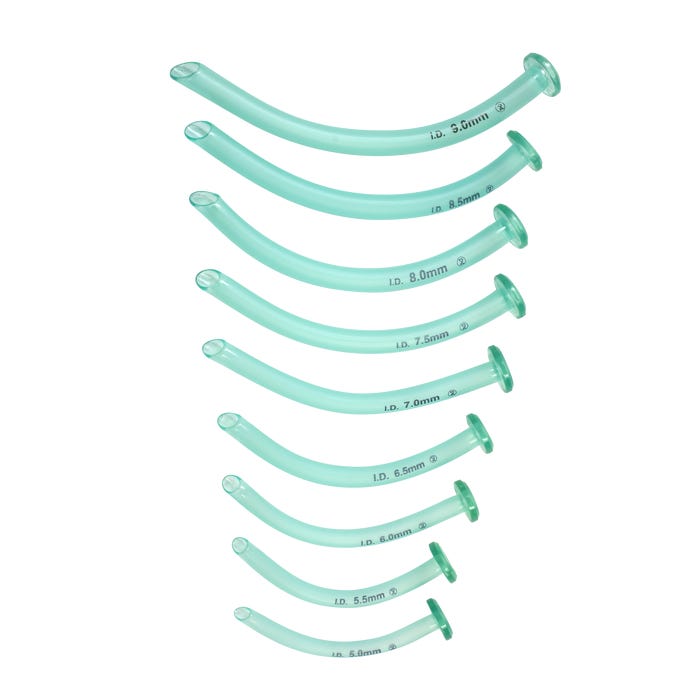
Oropharyngeal airway: One cannot use an oropharyngeal airway in patients with a severe gag reflex or oral trauma, as it could stimulate this gag reflex and lead to aspiration of gastric contents. Different sized oral appliances are available. They are measured and sized from the lip to the angle of the jaw and are useful for patients with spontaneous respirations who need help to keep their airway open.
Nasopharyngeal airway: This is used in patients with an intact gag reflex, trismus, or oral trauma, or those who have undergone oral or oropharyngeal surgery where the oral cavity should not be instrumented. The important factor in sizing a nasopharyngeal airway (NPA) is not only the tube’s width (which may be dictated by nostril aperture diameter or nasal septal and turbinate position) but also the stature of the subject.
A study of 413 infants under 12 months found an association between subject height and nares-vocal cord distance. To place the NPA in infants, the insertion length must, therefore, be slightly less than the anthropometric measurement of nose tip-earlobe distance.
Bag-mask Ventilation
A properly performed mask ventilation is the fundamental maneuver in airway management. Both in adults and children, there are one- and two-hand techniques. For neonatal airway, one hand technique is usually effective, as a single hand can often perform all necessary maneuvers. One can relieve the upper airway obstruction encountered during simple mask ventilation via head tilt, chin lift, jaw thrust, and the application of continuous positive airway pressure. Bag-mask ventilation is also appropriate while preparing to intubate.
Advanced Airway
Examples are supraglottic devices (laryngeal mask airway, laryngeal tube, esophageal-tracheal) and endotracheal tube.
Laryngeal mask airway: A relatively recent advancement is the development of the supraglottic airway. Many devices exist. Two of the more popular supra-glottic devices, the classic laryngeal mask airway (LMA) and pro-seal LMA, have good data in the pediatric population to support their safety and efficacy. Children with a recent upper respiratory infection have an increased incidence of respiratory complications with the use of LMA as compared to healthy children. This facilitates the rapid establishment of a more secure airway, particularly in an emergent setting where emergency medical technicians or other personnel may be establishing a pediatric airway and may not be as comfortable in doing so.
Esophageal-Tracheal tube
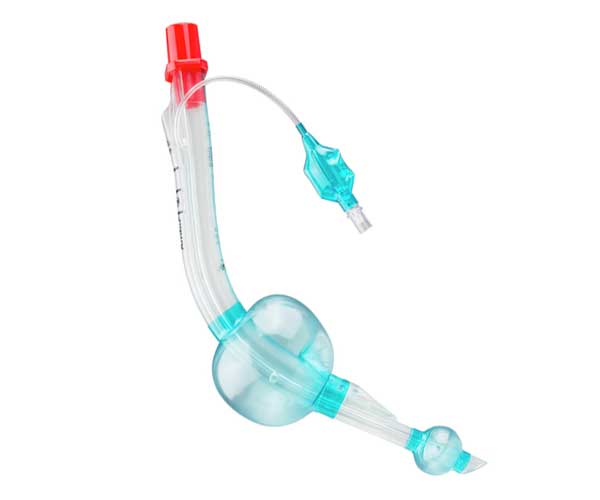
This is a supraglottic airway device now frequently used by many emergency medical personnel that intentionally intubates the esophagus, but the design of the device allows ventilation via a two-cuffed system and a ported tube. They are popular because of their ease of administration. They come in different sizes, but their routine use does not routinely extend to pediatric airway management.
Oxygen
Oxygen is a critical component of airway management. Pre-oxygenation with nasal cannulae, bi-valve mask, high flow oxygen, or bi-pap before the intubation can deliver the much-needed oxygen prior to intubation attempt.
Airway Management in Traumatic Patients
Trauma is a leading cause of morbidity and mortality worldwide, especially for people aged 15 to 50. Trauma is the second-most common single cause of death, representing 8% of all deaths. The World Health Organization estimates that traumatic injuries from traffic accidents, drowning, poisoning, falls, burns, and violence kill over five million people worldwide annually, with millions more suffering from the consequences of injuries.
Rapid evacuation and transportation to a trauma center improve the outcome of severely injured patients. Prehospital intubation is controversial in the EMS literature. The medical director of an EMS service will dictate the clinical context in which he/she will allow a paramedic to intubate in the field. The EMS service monitors and transports these patients quickly and safely to the nearest trauma facility.
