Naxalone
Published (updated: ).

Over the past two decades, the rate of overdose from opiates has increased significantly. While many factors have contributed to opioid overdose in the United States, the rate of overdose appears to be highest in rural communities compared to those living in urban areas. For example, in West Virginia, where over 50% of the population resides in rural areas, the state has the highest per-capita overdose rate compared to any other state. Opiate abuse is associated with enormous morbidity and mortality; people are reportedly overdosing on opioids nationwide. Naloxone has been the only antidote to opioids for over 50 years, and the drug has been readily available as a parenteral formula. The belief is that naloxone acts as a pure mu-opiate receptor competitive antagonist. There is no question that naloxone is of great benefit in preventing the accidental overdose from opioids. Because of this property, the federal government has now recommended that the drug be readily available as an over-the-counter formula in most pharmacies. Naloxone is available without a prescription in 43 states. Besides being available in hospitals, the drug is carried by emergency medical staff as well as law enforcement personnel. Also, the availability of naloxone over the counter has made it easier for family members and caregivers of patients with opioid use disorder to administer the drug. Unfortunately, there is little evidence to support the effectiveness of naloxone in preventing illicit opioid abuse. Healthcare workers feel that to counteract the opiate epidemic, the government should be focusing more on education, awareness, and safer alternatives than making naloxone empirically available for use by non-healthcare professionals.
Indications
Naloxone is indicated for the treatment of opioid toxicity, specifically to reverse respiratory depression from opioid use. It is useful in accidental or intentional overdose and acute or chronic toxicity. Common opioid overdoses treated with naloxone include heroin, fentanyl, carfentanyl, hydrocodone, oxycodone, methadone, and others.
Mechanism of Action

Naloxone is a pure, competitive opioid antagonist with a high affinity for the mu-opioid receptor, allowing for reversal of the effects of opioids. The onset of action varies depending on the route of administration but can be as fast as one minute when delivered intravenous (IV) or intraosseous (IO). It has a half-life of 30 to 120 minutes, depending on the route of administration, with IV being the fastest. In most cases of overdose, the reversal is observable in a matter of minutes. If no signs of reversal are apparent after administration of 10 mg of naloxone, one must consider co-ingestants like the tricyclic antidepressants, alcohol, benzodiazepines, cocaine, methamphetamine, and club drugs
Administration
Naloxone administration is usually via IV, but if no IV access is available, it can also be administered via an IO line, subcutaneously (SQ), IM, or via the intranasal (IN) route. When administered IV, naloxone usually fully reverses the opioid effects within a few minutes. The dose is titrated to effect, with the goal to increase the patient’s respiratory drive to allow for adequate spontaneous respiration and oxygenation but not bring to full reversal, which can result in withdrawal and can include combative or aggressive behavior. A small initial dose, usually 0.04 mg to 0.1 mg IV, is recommended in opioid-dependent patients with symptoms of opioid overdose to avoid opioid withdrawal symptoms. Larger initial dosing, such as 0.4 mg IV, is recommended in patients without a known history of opioid dependency. In patients who present apneic or near-apnea with cyanosis, especially in the prehospital setting, providers should not hesitate to give larger initial doses, such as 1 mg to 2 mg IV or 2mg intranasal, IM, or SQ. Clinicians can administer subsequent doses of 0.1 mg to 0.4 mg IV or 0.4 mg to 1 mg NAS, IM, or SQ in any opioid overdose patient until reaching the desired effect.
Continuous Intravenous infusion (Off-label)
Some patients may have overdosed on long-acting opioids like methadone, and in such cases, an intravenous drip of naloxone may be useful. In general, one can use two-thirds of the initial effective dose of naloxone (0.1 to 6 mg/hr) as a bolus every 60 minutes, or one can administer one-half of the initial bolus dose 15 minutes after starting the continuous IV infusion; this maintains a consistently high dose of naloxone.
Endotracheal Administration
Although emergency medical personnel and emergency healthcare workers often administer naloxone via the endotracheal tube, there is little evidence to support the effectiveness of this mode of administration. In dire circumstances with a patient in extremis, there may be no other choice, with doses of naloxone from 0.8 to 5 mg used.
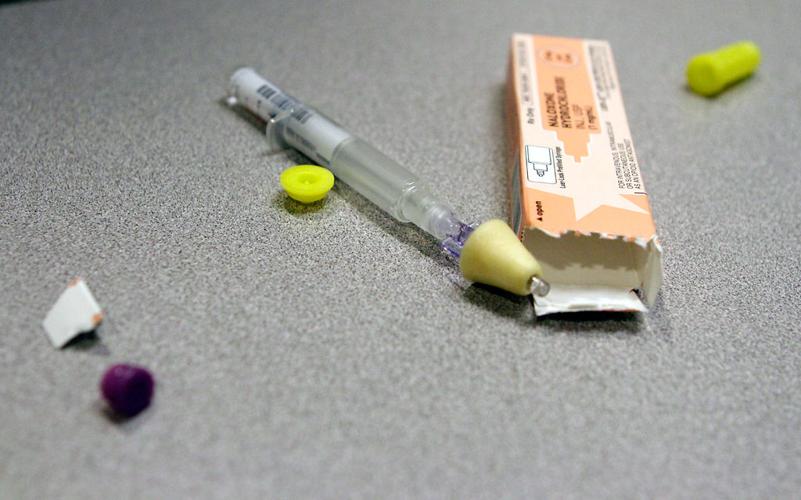
Intranasal Spray

Recently, the FDA approved the intranasal spray (NAS), which is available as an autoinjector. This device delivers 4 mg of naloxone and is usable by caregivers or family members. Initially, one spray is administered, which provides 4 mg of naloxone. Since the NAS is a recommended intervention for non-healthcare professions, there are a few recommendations when using this agent to reverse opiate overdose:
- Immediately following the administration of the first NAS, one should seek emergency medical assistance and not assume that the patient is fine, even if full mental recovery occurs.
- The individual requires close monitoring for his or her vital status, and repeat dosing may be necessary. If the patient relapses and the respiration rate decrease before emergency medical personnel arrive, administer the second dose.
- If repeat dosing is necessary, then it should be administered in alternate nostrils every two to three minutes.
- If the patient fails to respond to additional doses, then one must be prepared to perform other resuscitative maneuvers, including CPR.
The key reason for the development of the NAS formula is to permit medically untrained individuals to safely administer naloxone with a good probability of reversing the opioid-induced respiratory depression, especially if the patient has labored and shallow breathing. Unlike the parenteral route of administration, there is no need to worry about the accessibility of the peripheral veins, needlestick injuries, or disposal of sharps. However, even though NAS naloxone campaigns are widely promoted in most states, the pricing of this formula is still a major issue and might be a deterrent to widespread acceptance. Until a low-cost alternative is available, some consumers may not buy this product because of its expense, and the opioid epidemic will continue unabated.
Dosage Modifications
Partial opioid agonists or mixed agonist/antagonists
If the patient has overdosed on longer-acting opioids or partial agonists (e.g., buprenorphine, pentazocine), the recovery may be incomplete, and one requires higher doses of naloxone or repeated administration. Repeat dosing of naloxone can be done every two to five minutes. However, in some cases, the patient may benefit from an IV drip of naloxone.
Dosing Considerations
Intended for immediate administration of emergency therapy in settings where opioids may be present
It is vital not to assume that naloxone is the only treatment for opioid overdose. Naloxone is not a substitute for emergency medical care.
Providers should be aware that redosing of naloxone may be required. Given the presence of synthetic opioids, such as fentanyl or carfentanil being implicated more in overdoses, providers should prepare to deliver larger total doses, upwards of 10 mg, of naloxone. This fact was highlighted in a recent paper out of Jackson Memorial Hospital in Miami, Florida. At their institution, there was a 119% increase in opioid overdoses over three-months in 2016 compared to the same three months the previous year. There was a disproportionate increase in the amount of naloxone administered to patients during this period with the number of naloxone vials used increasing by 476%. The thinking was that due to a more potent synthetic opioid, such as fentanyl, being present in the heroin circulating through the area in 2016 compared to more traditional heroin in 2015.
For those patients in the emergency department who have required multiple doses of naloxone and are under consideration for admission, a continuous naloxone infusion may be necessary. The typical dose for this infusion is determined by calculating the wake-up dose needed for the patient and administering two-thirds of that dose per hour via continuous infusion.
If the patient fails to respond to repeated doses of naloxone, one must consider other causes of unconsciousness. After the acute treatment of the overdose, the patient should be enrolled for substance abuse treatment and encouraged to enter rehabilitation.
Adverse Effects
Naloxone has few side effects. The most common are those of acute withdrawal from opioids, such as anxiety, aggression, nausea, vomiting, diarrhea, abdominal pain, and rhinorrhea. In rare cases, the use of naloxone can precipitate noncardiogenic pulmonary edema. The incidence of naloxone-induced noncardiogenic pulmonary edema is estimated to be between 0.2% and 3.6% of patients who have received naloxone and are transported to the emergency department. Symptoms include persistent hypoxia, despite the resolution of respiratory depression secondary to acute overdose. Patients may also have a cough productive of the classic “pink, frothy sputum” indicative of pulmonary edema. Chest radiography will be consistent with the findings of pulmonary edema. It bears mention that the onset of noncardiogenic pulmonary edema occurs within 4 hours in most patients. However, there have been case reports of delayed onset of up to 8 hours after naloxone administration.
Contraindications
There are no absolute contraindications to the use of naloxone in an emergency. The only relative contraindication is known hypersensitivity to naloxone.
Monitoring
Patients who overdose on opioids can have not only respiratory depression but also hypotension. These patients should be resuscitated like any other patient and monitored. Additionally, naloxone administration also can trigger an acute withdrawal syndrome, which can present with the following symptoms:
- Nausea
- Diaphoresis
- Vomiting
- Tachycardia
- Cardiac Arrest
In chronic opioid users, naloxone requires slow administration to individuals who are dependent on opioids. All patients who have responded to naloxone should be continuously monitored for at least six to 12 hours since some opioids (methadone, fentanyl, buprenorphine) have a much longer half-life than naloxone. The half-life of naloxone in adults varies from 30 to 80 minutes. The patient should have vital signs, including pulse oximetry, monitored until obtaining a full recovery. Even after reversing respiratory depression, the patient must be monitored for at least six to 12 hours because the patient may have ingested the longer-acting opioids, which will continue to exert their effects after excretion of the naloxone. Any patient that requires IV naloxone of doses more than 5 mg should be admitted.
For those who completely reverse with 0.4 to 2 mg of naloxone, observation in the emergency room for two to four hours is prudent. If the patient is stable, then discharge is recommended. In general, patients considered for discharge after reversal of the opioid overdose with naloxone should:
- Be fully mentally alert with a Glasgow coma scale of 15
- Not require further dosing of naloxone in the emergency
- Have an oxygen saturation of at least 92% on room air
- Have a respiration rate of no less than ten breaths per minute
- Have a pulse rate of no less than 50 or no more than 120 beats per minute
- Have a blood pressure between 110/90 to 140/90 mmHg
- Be able to tolerate clear liquids, ambulate, and have no withdrawal symptoms
- Have someone drive the patient home and monitor the patient for the next 12 to 24 hours
Contraindications
There are no absolute contraindications to the use of naloxone in an emergency. The only relative contraindication is known hypersensitivity to naloxone.
Current Guidelines
Because of the current opioid epidemic, recent legislation has been passed in the United States that allows physicians to prescribe naloxone to opioid abusers to reverse the overdose. Also, more than a dozen states have passed good Samaritan laws that permit healthcare workers to prescribe naloxone to the family members or caregivers of opiate abusers. There are now campaigns across the nation to make naloxone easily available to the public, firefighters, police, and other professionals.
Out of hospital use
Although naloxone is effective in reversing opioid overdose in a hospital setting, its use out of the hospital is relatively new. Thus not much data are available on its effectiveness. Overall the NAS formula is less effective than the parenteral formulations. Further, there are no studies that have compared the different routes of administration, the timing of the response, and titration strategies.
Naloxone storage

Naloxone is stored at room temperature and contained in a protective outer case. This type of packaging makes the product impact-resistant and easy to transport in the ambulance.
Many patients who are addicted to opioids are also prescribed naloxone and may inject the antidote if they feel they have overdosed for home use; the NAS formula is preferred because it eliminates the risk of accidental needle sticks with a contaminated syringe or needle. Plus, the NAS formula avoids the difficulties with the disposal of needle and sharps.
Discussion
Even though naloxone has already saved many lives, the general feeling in the medical community about its universal availability remains debated. Some medical experts suggest that making naloxone available over the counter may promote more use of opioids. Further, some experts feel that the ready availability of naloxone will lead the opioid user to start abusing higher doses more frequently because they know that an antidote is readily available if anything happens. There are also concerns that the average person lacks the training to make a diagnosis of an opioid overdose, and this could lead to misuse of expensive medication. Further, once the pharmacological effects of naloxone have worn off, there is a possibility that respiratory depression may recur, and without monitoring, this could spell real trouble for the patient. Finally, because naloxone is readily available, bystanders may be less reluctant to call for emergency assistance since they may think that the individual has achieved full recovery from the overdose.
