Aspirin
Published (updated: ).

Salicylates have been available since the early 1900s. Salicylates have been derived from the willow tree bark. The Sumerians were noted to have used remedies derived from the willow tree for pain management as far back as 4000 years ago. Hippocrates used it for managing pain and fever. He even utilized tea brewed from it for pain management during childbirth.
In a 1763 clinical trial, the first of its kind, Reverend Edward Stone studied the effects of willow bark powder for treating fever. About 100 years later, the effects of the willow bark powder were studied for acute rheumatism.
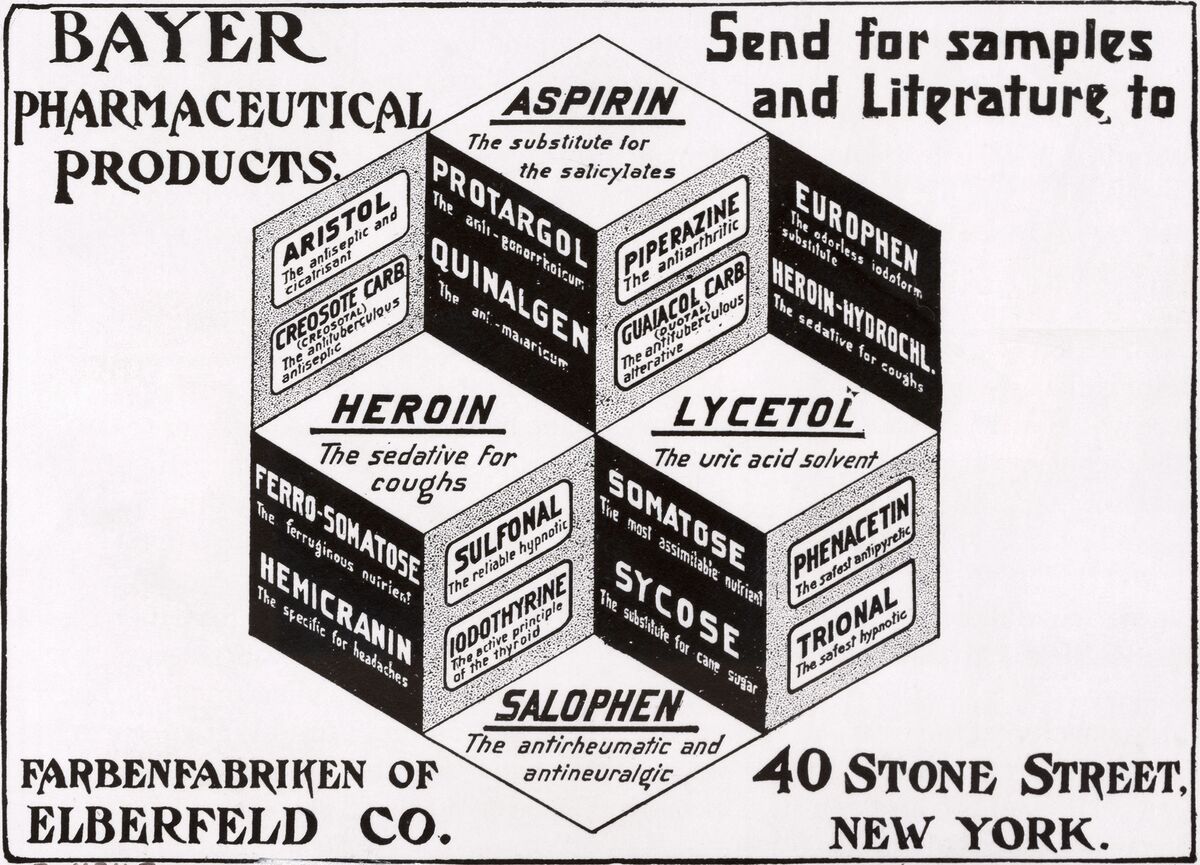
In 1828, Professor Johann Buchner used salicin, the Latin word for willow. Henri Leroux used it to treat rheumatism after isolating it in a crystalline form in 1829. In the 1800s, the Heyden Chemical Company was the first to mass-produce salicylic acid commercially. It was not until 1899 when a modified version named acetylsalicylic acid was registered and marketed by Bayer under the trade name aspirin.
Even though it has been available since the early 1900s, its real mode of action was not known until the late 1970s. Some of the indications for aspirin use are as follows:
- Angina pectoris
- Angina pectoris prophylaxis
- Ankylosing spondylitis
- Cardiovascular risk reduction
- Colorectal cancer
- Fever
- Ischemic stroke
- Ischemic stroke: Prophylaxis
- Myocardial infarction
- Myocardial infarction: Prophylaxis
- Osteoarthritis
- Pain
- Revascularization procedures: Prophylaxis
- Rheumatoid arthritis
- Systemic lupus erythematosus
Mechanism of Action
Aspirin is a cyclooxygenase-1 (COX-1) inhibitor. It is a modifier of the enzymatic activity of cyclooxygenase-2 (COX-2). COX inhibitors are medications used in the management and treatment of chronic pain syndromes. They are in the anti-inflammatory class of drugs. Unlike other NSAIDs (ibuprofen/naproxen), which bind reversibly to this enzyme, aspirin binding is irreversible. It also blocks thromboxane A2 on platelets in an irreversible fashion preventing platelet aggregation.
Blood clots are formed through the process of hemostasis. In primary hemostasis, platelets activate and aggregate to form a platelet plug. This platelet plug is then strengthened by fibrin and a thrombus is formed during the process of secondary hemostasis. Hemostasis is essential to prevent excessive loss of blood. However, when a thrombus forms inside an artery, it blocks the flow of blood to that tissue. This causes a myocardial infarction, if a coronary artery supplying blood to the muscle of the heart is blocked, or a stroke, if a thrombus forms in an artery supplying blood to the brain. In high-risk patients, it is critical to prevent the formation of thrombi in these arteries. This is where aspirin becomes helpful.
Aspirin prevents thrombi formation by blocking platelet production of thromboxane A2, an essential platelet aggregation component. Aspirin has the ability to suppress the creation of prostaglandins and thromboxane A2 by irreversibly inactivating the cyclooxygenase-1 (COX-1) enzyme. COX-1 plays an important role in prostaglandin and thromboxane
Administration
Aspirin can be administered via the oral, rectal, and intravenous (IV) route.
It is available in different doses, the lowest being 81 mg, also called a baby aspirin.
- Tablet: 325 mg, 500 mg
- Delayed-release tablet: 81 mg, 325 mg, 500 mg, 650 mg
- Chewable: 81 mg
- Suppository: 60 mg, 120 mg, 200 mg, 300 mg, 600 mg
- Intravenous: 250 mg, 500 mg
Pharmacokinetics
Aspirin absorption from the gastrointestinal (GI) tract depends on the formulation state. When consumed as a liquid preparation, it is rapidly absorbed as opposed to tablets. Its hydrolysis yields salicylic acid. Salicylic acid has a narrow therapeutic window. If maintained within that narrow range, it provides the appropriate anti-inflammatory effect.
Aspirins absorption is pH sensitive at the level of the small intestine. Absorption is higher through the small intestine than the stomach for the same pH range. At pH 3.5 or 6.5, aspirin’s intestinal absorption is greater than the gastric absorption of the compound. The stomach does not absorb aspirin at pH 6.5.
Salicylate elimination occurs through two pathways via the creation of salicyluric acid and salicyl phenolic glucuronide. Salicylic acid is renally cleared, which can be increased by raising the urinary pH. Medications like antacids can increase renal clearance as they raise urinary pH. It can cross the blood-placental barrier. It is also expressed in breast milk.

Adverse Effects
Aspirin has had multiple metanalyses, which suggest that aspirin reduces the risk of major adverse cardiovascular events in patients who have diabetes without cardiovascular disease while also causing a trend toward higher rates of bleeding and gastrointestinal complications. The most common side effect of aspirin is gastrointestinal upset ranging from gastritis to gastrointestinal bleed.
Hypersensitivity
Hypersensitivity to NSAIDs is common among the general population. The rate is about 1% to 2%. Symptoms could be as mild as a simple rash to angioedema and anaphylaxis. In patients with asthma or chronic rhinosinusitis, the prevalence of these allergic symptoms could be as high as 26%. If this is accompanied by nasal polyps and inflammation of the respiratory tract with eosinophils, it is called the aspirin triad. NSAID-exacerbated respiratory disease (NERD) is a new term associated with this syndrome due to upper and lower respiratory mucosal inflammation.
Reye Syndrome
Reye syndrome, named after the Australian pathologist Dr. R.D. Reye was first described in 1963. It is a rare but fatal condition with an estimated mortality rate of between 30% to 45%. It is a form of encephalopathy secondary to fatty changes in an otherwise healthy liver. The clinical vignette of Reye syndrome constitutes a viral upper respiratory tract infection in children and concomitant administration of aspirin for the treatment of fever. It is thought that mitochondrial injury secondary to the preceding viral illness is the first hit to both the liver and the brain. Aspirin or similar compounds provide the second hit completing the syndrome. The incidence has dramatically decreased due to better awareness and the use of acetaminophen to manage fever in children instead of aspirin.
Even though the association between aspirin and Reye syndrome exists, some authors argue that at the time of diagnosis, salicylate levels were not routinely checked, biopsies were not obtained, and genetic/inborn errors of metabolism were not ruled out.
Aspirin increases the risk of intracranial bleeding (RR = 1.65; 95% CI, 1.06 to 5.99) versus placebo.
Contraindications
People who are allergic to ibuprofen should not take aspirin as there is cross-reactivity. Patients who have asthma should be cautious if they have asthma or known bronchospasm associated with NSAIDs.
Aspirin increases the risk of GI bleeding in patients who already suffer from peptic ulcer disease or gastritis. The risk of bleeding is still present even without these conditions if there is concomitant alcohol consumption or if the patient is on warfarin. Patients who have inborn coagulopathies such as hemophilia should avoid all salicylates. Acquired diathesis as in the setting of dengue or yellow hemorrhagic fever should avoid the use of aspirin.
Patients who have glucose-6-phosphate dehydrogenase deficiency are at risk of acute intravascular hemolytic anemia. Many factors can precipitate these hemolytic episodes. Aspirin is one such know cause.
Avoid using aspirin in children who are suffering from a viral infection to avoid Reye syndrome.
