Decompression Sickness
Published (updated: ).
Introduction

As any person ventures into an increased pressure environment, they begin to absorb the inert gasses in their breathing media in proportion to the percentage of each gas inspired (Dalton’s law). In the air, the bulk of the inert gas is nitrogen (approximately 78%), and the gas is absorbed based on the amount of increased pressure and the time the individual inspires the gas. Functionally, this can be seen underwater, in deep tunnel drilling, in caissons, or in other exotic increased pressure environments. It is most easily conceptualized in a diver descending underwater, so that model will be used for this explanation.
Diving using an underwater breathing apparatus (UBA) of any type involves the inspiration of gas by the diver at ambient pressure, which is increased from normal surface pressure. Seawater is sufficiently denser than air that 1 atmosphere (atm) of air is equivalent to 33 feet of seawater (FSW), meaning the diver can double their ambient pressure by descending only 33 feet in the water column. As pressure increases, the amount of inert gas dissolved in the diver’s bloodstream and tissues also increases, which exponentially decreases the time the diver can remain at depth without taking time to off-gas (decompress) prior to returning to the surface. Divers who remain at depth past the no-decompression time limit for that specific depth are at increased risk of the dissolved inert gas in their bodies reaching a critical supersaturation point during their ascent and having gas bubbles form de novo either in the bloodstream or in tissues. These bubbles are often asymptomatic but can result in decompression sickness when the gas bubbles themselves do damage to the surrounding tissues.
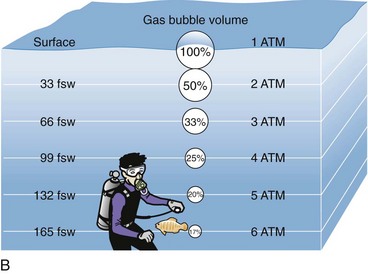
Because the amount of dissolved gas is related to the time as well as the ambient pressure increase, it is necessary to address both components. As depth increases, the probability of decompression sickness increases exponentially. A diver at 15 feet of saltwater, typically, can stay indefinitely with almost no chance of decompression sickness while a diver at 60 feet can only remain for about an hour before needing to stop and decompress prior to direct return to the surface. The same diver at 100 feet of saltwater would only have 25 minutes and only about 5 minutes at 150 feet. Once a diver remains beyond these limits, direct return to the surface would mean a statistically significant increase in the probability of decompression sickness via bubble formation in the bloodstream or tissues and must be mitigated with stops on the way back to the surface to provide the diver with the opportunity to breath out inert gas and thereby prevent bubble formation. Once bubbles have formed and then become symptomatic, recompression is required for resolution. Recompression in a chamber is safest, but if recompression in a chamber is unavailable or will be delayed many hours due to travel time, recompression in the water can be considered.
Divers experiencing decompression sickness (DCS) require recompression on pure oxygen to dissolve the gas bubbles in their blood and tissues, allow excess nitrogen to diffuse out, and oxygenate ischemic tissues, thereby treating the disease process. Recompression has classically been achieved with a special chamber allowing a controlled increase in ambient pressure as well as a treating physician or technician to care for the stricken diver. There has been an alarming decrease in the number of recompression chambers available for 24-hour emergency care across the nation, resulting in divers with DCS facing long transit times to available chambers. This delay in care negatively affects the diver’s probability of complete recovery, resulting in many divers considering the alternative known as in-water recompression (IWR). IWR involves intentionally placing the stricken diver back in the water on pure oxygen, typically with a prolonged oxygen-breathing period at 30 FSW or less, with a gradual ascent to the surface. In water, recompression has been used for decades by several navies throughout the world as well as globally in remote areas where local recompression chambers are simply not available. The Australians developed and have used a relatively standardized protocol for several years, as has the United States Navy for use in extraordinary circumstances, as it is normal navy policy to have a chamber on-site for diving operations.
Function
Both the United States Navy and Australian protocols have been used extensively and offer a significant chance of improvement in symptoms and resolution of symptoms, but all in-water recompression techniques share similar limitations. In all cases, careful evaluation of the diver to determine the diver’s suitability for return to the water must be made. Divers who are paralyzed or have an alteration of their mental status should generally not be recompressed in the water due to the potential for drowning. Divers should always have a tender enter the water with them who is capable of rescuing the injured diver should their decompression sickness progress include paralysis. A sufficient amount of oxygen should be available to complete the treatment, with a suitable reserve to ensure that the diver can be fully treated and egress the water safely. Thermal protection also is important, as the diver may already be cooled from the dive prior to the injury. Diver cooling sufficient to change perfusion of tissues increases the probability of decompression sickness and is a significant concern, even in relatively warm (80 to 82 degree) Caribbean waters and much more so in cooler waters prevalent throughout the diving world. Additional environmental concerns such as high currents or the presence of dangerous marine life must also be taken into account.
Recompression in the water should only be considered with the following resources:
- Adequately trained divers, both the stricken diver and the tender
- The availability of enough oxygen to complete the treatment with adequate reserve
- The availability of a safe in-water site to conduct the recompression
- The availability of equipment such as full face masks (communications are desirable but can be accomplished with hand signals and slates), diver tethers, and a downline at a minimum
- Adequate thermal protection for the diver and tender
- Diver evaluation to ensure there are no contraindications to going in the water (clinical hypothermia, paralysis, altered mental status, or cardiopulmonary instability)
- Divers with urinary retention or abdominal pain should be recompressed with care, as these symptoms often herald worsening spinal decompression sickness, which can progress to paralysis. Conversely, these are the divers who may benefit most from in-water recompression.
Issues of Concern

Decompression illness (DCI) is the entire subset of possible decompression-related maladies and includes two principal categories: (1) decompression sickness, which is a constellation of maladies that result from bubble formation due to dissolved gas coming out of solution with a decrease in ambient pressure and (2) overexpansion injuries (including arterial gas embolism/AGE), which result from gas of any kind expanding directly due to the effect of Boyle’s law as ambient pressure is reduced. Diving injuries of any kind are rare, with the current incidence of diving maladies overall varying from 1 to 3/10,000 dives. Most evidence indicates that the incidence of arterial gas embolism is at least an order of magnitude less common, implying an incidence of fewer than 1/100,000 dives. Accident rates for deeper mixed gas and rebreather dives, especially those involving wreck and cave diving, are generally accepted to be higher, but the accident rate has never been accurately totaled, and the number of these dives made per year is completely unknown, making the published rate statistics unreliable at best. It is not known how many of these accidents would respond to IWR, but it has been observed in many studies that a short time interval to recompression is associated with both better outcomes and decreased morbidity.
Decompression sickness (DCS) can manifest in an almost limitless number of ways, as the disease is caused by bubble formation and subsequent tissue damage and can occur at any place in the body. Type 1 DCS is typically joint or muscle pain and from direct bubble insult. It typically responds well to recompression, and complete recovery is common. By definition, any involvement of the cardiac, pulmonary, central nervous system, or lymphatic system is type 2 DCS and is more severe. Type 2 DCS can manifest as cardiopulmonary instability, hypoxia, confusion, partial or complete paralysis, or even crossed neurological deficits, as the insult is caused by bubbles rather than a single thromboembolic event. Subtle presentations of neurological DCS can occur with sudden onset ataxia, vertigo, or personality changes. While sudden-onset neurological findings should be fully evaluated, the recent history of ascent from a dive greater than 33 FSW should prompt consideration of DCS. The ascent from a dive to any depth, however trivial, while breathing compressed gas can result in overexpansion injuries and arterial gas embolism (AGE). Both AGE and DCS can present with neurologic symptoms and require recompression therapy but are most easily distinguished by the presence of unconsciousness within 10 minutes of surfacing that is considered highly predictive of AGE. The subtle nuances between these injuries and the complexity of treatment options are best evaluated by a physician trained in undersea and hyperbaric medicine. Confirmed or suspected cases of AGE are generally not good candidates for IWR due to their syncope and often hard neurological deficits that would place a diver returning to the water at great risk.
There are no lab or radiographic findings that are pathognomonic for decompression illness. A chest x-ray is advisable if it does not delay recompression at a facility, but there is no pre-dive workup needed prior to in-water recompression save a documented neurological exam by the most competent provider present and a blood glucose level in a patient with known diabetes. Rescue divers and instructors are trained to perform and document a 5-minute neurological exam as part of the DCI evaluation. In the field, this evaluation is sufficient. At the hospital or emergency department, physicians are advised not to unnecessarily delay recompression but also to remember that today’s aging diver population has all the same pathology as anyone else presenting to the emergency department. While DCI should always be in the differential for anyone presenting after significant decompression stress, early anchoring should be avoided and a broad differential considered. Dives shallower than 33 feet are unlikely to cause DCS, and an alternate diagnosis should be explored in these cases.
History from the patient will be either consistent with a decrease in ambient environment pressure such as surfacing from a dive, decompression of a plane, or a spacecraft. The diver will often delay in presenting, as symptoms can be subtle initially and are often similar to musculoskeletal strain commonly encountered in the diving environment while moving heavy equipment. Once a diver and evaluator decide that DCS is likely and that recompression in a chamber will be delayed many hours or days, consideration of in-water recompression is appropriate. While no firm guidelines are provided by current research, most divers consider an expected delay of 8-12 hours or more from symptom onset to be sufficient reason to consider IWR. The decision to proceed with IWR should be based on both the severity of the DCS and the time to travel to a chamber. A full neurological exam should be documented to facilitate tracking the efficacy of the therapy and the need for future therapy. A quick cardiopulmonary exam is advised if that is possible on site, and the diver should be evaluated by history for signs of dehydration and hypothermia.
For older divers with an unclear history or symptoms typical of other disease processes, normal emergency evaluation is appropriate. While there are no controlled studies, isolated, dense stroke syndromes pathognomonic of single-vessel lesions should be rapidly investigated to determine etiology. A patient presenting with symptoms classically associated with a left middle cerebral artery infarct, for instance, is unlikely to have had bubble formation truly limited to a single vessel, while a diver with crossed, vague, and varied neurological complaints likely has DCS. Chest pain and dyspnea can be the direct result of DCS and/or overexpansion injuries but can also herald acute coronary syndrome or pulmonary embolism. The emergency physician should perform an electrocardiogram (EKG) and obtain a laboratory workup, but not delay recompression. Holding a patient for serial cardiac markers who has a history consistent with decompression illness is as inappropriate as failing to perform an EKG on a patient with chest pain. If there is any question that the symptoms may not be dive-related, patients in the field should proceed to the nearest emergency department for evaluation and treatment. Medical transfer to a chamber is always possible if the injury is determined to be DCS, and the emergency department can provide stabilizing treatment for all conditions.
Clinical Significance
In-water recompression is a clinically significant mechanism to address a global lack of coverage for recreational, scientific, and exploration divers who often find themselves many hours, or even days, from the nearest chamber. Multiple studies have demonstrated that time to recompression is directly related to decreased morbidity, and presumably, mortality. Divers with severe DCS with the appropriate resources and training can treat their decompression sickness on-site, allowing for non-emergent transfer and evaluation and even ongoing treatment. In addition to potentially preventing long-term disability, the cost savings and risk reduction to rescue personnel for an unplanned and emergent evacuation from a remote area can be significant. In-water recompression with trained divers is a viable alternative when safe and rapid transfer to a dedicated recompression chamber is not feasible.
Other Issues
Australian and United States Navy IWR tables are similar in that they both require in-water recompression to 30 feet and approximately 60 to 90 minutes at 30 feet, with about an hour at 20 and 10 feet, respectively. Neither table provides a deeper excursion or significant modification of the treatment in the water by the diver or tender. Both tables have the tender breath air during the treatment protocol for safety reasons, thereby preventing oxygen-induced seizures at the same time in both the tender and stricken diver. Having the tender breath air also allows for simplified logistics, as all the onsite oxygen is available to the stricken diver.
Summary Points
- Use only pure oxygen for IWR unless alternate treatment strategies are approved by a hyperbaric physician specifically trained in undersea medicine.
- Have an adequate supply of oxygen before initiating IWR.
- Have proper equipment and training before IWR is needed in an emergency.
- Properly evaluate the diver and situation for suitability for IWR.
- Utilize tables with a clear history of success in treating divers.
- Never send a stricken diver into the water alone.
