Snake Bites
Published (updated: ).
Introduction
Snakebites are responsible for a significant degree of morbidity and mortality worldwide, especially in low resource countries. There are over 600 identified species of venomous snakes worldwide, with the majority belonging to the Viperidae and Elapidae families. Common names among the Viperidae family are vipers, pit vipers, and adders. Distinguishing features of the Viperidae family include long, retractable fangs, triangular heads, elliptical pupils, and small scales on their tails. The pit vipers also have a heat-sensing pit adjacent to their nares for movement detection to aid in hunting prey.
Etiology
Snake envenomation worldwide is primarily related to occupational exposure, such as in farmers and hunters, but is also seen among tourists exploring the outdoors. When snake envenomation occurs in humans, the initial damage is local around the site of the bite and may spread to systemic toxicity depending on the species.
Snakes primarily use their venom production for targeting prey, but it is also a form of self-defense. Some species can selectively release their venom leading to the occurrence of “dry bites,” in which there is the delivery of no venom. When venom gets released with their bite, the overall toxicity is dependent on both the volume of the venom released and the median lethal dose (LD50) of the venom.
Epidemiology
There are an estimated 1.2 to 5.5 million people affected by snake bites worldwide each year, with as many as 94,000 of these leading to death. The regional variation is quite staggering with only five snakebite related deaths occurring in the United States in comparison to India, which has one of the world’s largest number of snake bites annually, with an estimated 50,000 snakebite related death. The cause of this variation is twofold. The first being a higher prevalence of venomous snakes in a more densely populated region with poorer living conditions. The second factor is that the access to healthcare in these regions is limited with long travel times to reach a suitable treatment center and lack of antivenom availability. Within the United States, the vast majority of snake envenomations occur in the southwest states with envenomations from the Viperidae family. Children only comprised 28% of envenomations, and males were more likely to be victims at 59%.
Pathophysiology
The symptoms seen from snake envenomations are mainly due to the toxic components in their venom. The exact composition ranges from species to species and can vary significantly from localized tissue destruction to profound coagulopathies. The clinical effect on humans is related to both the potency and the volume of the toxin released during the snake bite. The venom released by the inland Taipan from Australia is the most potent in the world with a lethal dose of only 0.01 mg/kg with an average envenomation of 44 mg. Their envenomations have greater than 80% mortality.
Toxicokinetics

The composition of snake venom from a single species of venomous snake can consist of up to 100 different toxic elements. Local tissue destruction is primarily due to hyaluronidase and proteolytic enzymes in the snake venom, which can lead to local tissue edema, blistering, and tissue necrosis. There are a variety of other proteins and polypeptides with toxic effects, such as neurotoxins and hemotoxins. Most of the neurotoxic effects are secondary to damage at both the presynaptic and postsynaptic terminals of the neuromuscular junction. There are a wide variety of hemotoxins with effects on the coagulation cascade, platelet activation, and fibrin clot formation.
History and Physical
A detailed history of a patient suspected of having a snakebite is essential to delineate treatment options moving forward. Information to obtain includes the timing and location of the bite, the onset of any symptoms the patient has been experiencing, and any first aid administered in the field. Gathering a past medical history with detail to which medications they are on, specifically anti-platelet and anti-coagulant medications, and any allergies that would prohibit them from receiving an antivenom, such as horses. If possible, information on the offending snake should be gathered. Factors that contribute to the severity of the bite include size of the victim, with larger patients doing better, part of the body bitten, exertion following the bite, depth of the bite, species of snake causing the bite, time to the presentation at the hospital, and initial first aid given at the scene.
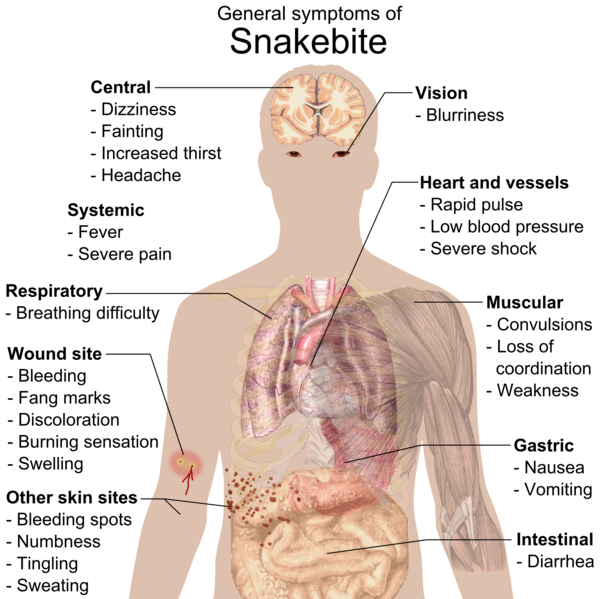
The physical exam may or may not reveal fang marks at the injury site. There could be local tissue damage, such as ecchymosis, blistering, or even tissue necrosis. Neurotoxic effects will initially present with generalized weakness, ptosis, and ophthalmoplegia; this may progress to paralysis of the facial muscles, and eventually, respiratory failure secondary to obstruction or paralysis of the diaphragm. Significant bleeding from the puncture site, epistaxis, or evidence of spontaneous bleeding could indicate a hemotoxic effect. Patients may present with signs of shock secondary to venom-induced vasodilation, hypovolemia, or even anaphylaxis in some patients.
The physical exam could help indicate the species of snake inflicting the bite. In general, Elapid bites are associated with minimal local tissue damage and have a neurotoxic syndrome with systemic toxicity. Viperid bites are associated with profound local tissue damage and have a hemotoxic syndrome with systemic toxicity.
Symptoms that may suggest systemic effects of the envenomation include nausea, vomiting, abdominal pain, lethargy, muscle weakness, muscle fasciculation, and severe headache. It is important to recognize these symptoms early to prompt initiation of antivenom administration.
Treatment / Management Or What Not To Do

The initial first aid at the scene should be minimal and aim at getting the patient to the nearest treatment center quickly. Varying opinions exist regarding the usefulness of placing the affected extremity in a splint and keeping it at heart level. Therefore, this should only occur if it will not delay transportation. Removal of jewelry and any constrictive clothing on the affected limb is necessary due to the possibility of swelling and circulatory compromise. The patient should be kept calm and encouraged not to exert themselves as this could increase the snake venom absorption. The primary concern of the medics is the possibility of anaphylaxis which can be easily treated with epinephrine.
Pressure bandages are another controversial topic. If the identity of the snake species is known to cause neurotoxicity and no local tissue damage, the application of a pressure bandage could slow the spread of the venom. However, if the venom is known to cause local tissue damage, the implementation of the pressure bandage may worsen the damage inflicted to the extremity. Application of a tourniquet proximal to the bite results in higher morbidity without any improvement in outcomes, so this practice has been discouraged. The use of venom extractors has also demonstrated to be ineffective. Local wound manipulation, such as incision or washout, is generally not suggested. Submersion of the extremity in ice cold water is also not recommended.
In some areas, measurement of the progression of swelling form Crotalidae (rattlesnake or copperhead) envenomation is essential to decide if antivenom is indicated. Place ink mark on the proximal edge of the bite swelling as a baseline for serial measurements. Mark the progression of swelling with a skin marker, noting the time. Measure the circumference of affected extremity at the same level each time (i.e., mid-forearm or mid-shin). Measure the swelling extension and record circumference every 15-30 minutes. Once there has not been any progression of edema after four consecutive measurements, then decrease measurement frequency to every hour. Antivenom is indicated if swelling progressed beyond the bite site.
Identification of the offending snake species will help determine the appropriate antivenom treatment. There are two antivenoms against Crotalidae approved in the United States.
What Else Could It Be?
In the absence of an observed snake bite, alternative envenomation, such as scorpion, tick, or spider bite, should be considered based on the region. For patients with a neurotoxic syndrome, one must consider Guillain-Barre as an alternative. Tick paralysis can also produce similar symptoms.
Prognosis
The majority of morbidity and mortality from snake bites are secondary to the toxin production associated with the bite. Patients who seek proper medical attention within the first 6 hours after the bite have significantly lower morbidity and mortality. Patients who are monitored and given supportive treatment during this period typically do not have any long-term side effects. Those with significant local tissue injury secondary to the snake envenomation may develop longstanding paresthesia, muscle damage, or even amputation in severe cases.
Complications
The primary complications from snake envenomations are due to the direct toxic effects. The localized tissue damage may require debridement or even amputation in severe cases. Reports exist of massive coagulopathies leading to profound blood loss. These coagulopathies usually resolve within 48 hours of the snake envenomation. Profound neuromuscular blockade can also occur, leading to pulmonary insufficiency if the diaphragm is involved. These symptoms also typically resolve within 72 hours of envenomation.
The administration of snake antivenom requires monitoring for signs of adverse reactions. These include an anaphylactic reaction that may occur within the first few minutes of administration and up to two hours. If a severe anaphylactic response is suspected, the infusion should stop, and the administration of epinephrine and an anti-histamine should follow. Patients may also develop a hypersensitivity reaction leading to pruritus, hives, nausea, and mild hypotension. This reaction may occur at any time during the antivenom administration and will dissipate once the infusion is complete. There are also documented cases of serum sickness as a side effect that may occur up to two weeks after administration. This usually presents as an influenza-like illness with a rash, and possible microhematuria. This condition responds well to a short course of antihistamines and oral corticosteroids.
