Cold Weather Injuries
Published (updated: ).
Cold weather-related injuries include: injuries due to decreased temperature (hypothermia, frostbite, nonfreezing cold injury), injuries due to heaters, carbon monoxide poisoning, and accidents due to impaired physical and/or mental function resulting from cold stress. Cold weather injuries can also occur in warmer ambient temperatures when an individual is wet due to rain or water immersion.
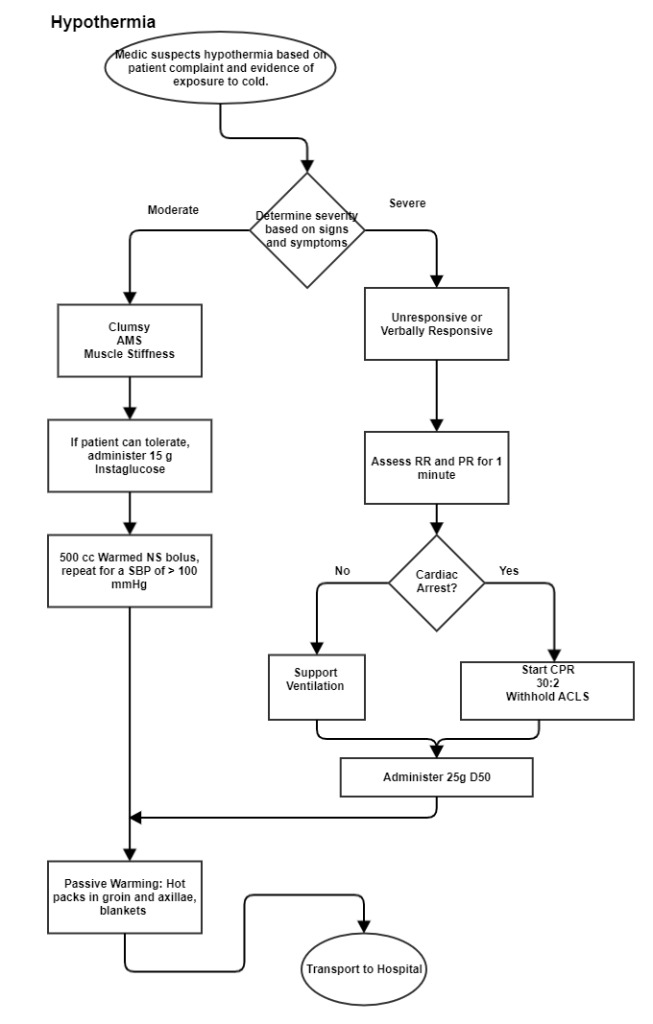
Hypothermia
Hypothermia is defined as a body core temperature below 95°F/35°C. Hypothermia is usually characterized as mild, moderate, or severe, based on body core temperature. In order to properly diagnose hypothermia, core temperature must be measured rectally with a thermometer with an extended low range scale. Oral and tympanic temperatures will not yield accurate results in a cold environment, even when care is taken to use the best technique.
Cause
- Hypothermia occurs when heat loss is greater than heat production. This can occur suddenly, such as during partial or total immersion in cold water, or over hours or days, such as during extended operations or survival situations.
- Hypothermia may occur at temperatures above freezing, especially when a person’s skin or clothing is wet.
Symptoms
- Vigorous shivering is typically present. Shivering may decrease or cease as core temperature continues to fall.
- Onset of hypothermia is typically associated with the so-called “umbles”, the grumbles, mumbles, stumbles and fumbles that increase as cold affects muscle and nerve function.
- Symptoms of hypothermia consist of confusion, sleepiness, slurred speech, shallow breathing, weak pulse, low blood pressure, change in behavior and/or poor control over body movements/slow reactions.
Prevention
- The keys to preventing hypothermia are layering clothing and staying dry. Remember the acronym COLD:
- Keep it Clean
- Avoid Overheating
- Wear it Loose and in Layers
- Keep it Dry
- Layers can be removed as ambient temperature or physical activity increases, which can reduce sweating and moisture build-up within clothing.
Treatment
- The goals for field management of hypothermia are to rescue, examine, insulate, and rapidly transport. If untreated, hypothermia is a true medical emergency and requires evacuation.
- Rewarming techniques include: Soldiers generating their own heat via shivering or exercise, insulating against further heat losses, use of heat on the skin and direct delivery of heat to the core. The latter can only be performed in a hospital setting.
- The use of external heat on the skin (radiant heat, hot water bottles, electric blankets) should only be applied to individuals who have ceased shivering or have a toxicological vasodilation that increases heat loss. Patients must be closely monitored and reassessed frequently to prevent burns.
- For most cases, moving the individual to a warmer location, replacing wet clothing and movement/light exercise are sufficient to restore core temperature.
Frostbite

Frostbite accounts for the largest number of CWI each year and occurs when tissue temperature falls below ~28-30°F. Frostbite can occur suddenly due to contact to cold metal or super-cooled liquids such as alcohol, fuel or antifreeze or can develop over time due to prolonged cold exposure. Frostbite is most common in exposed skin such as the hands, nose, ears, and cheeks but can also occur in the feet or in the hands while wearing gloves due to inadequate insulation and reduced skin blood flow.
Cause
- Exposure to below freezing temperatures (<32°F) causing freezing of skin, fingers, toes, ears and facial parts.
- Exposure of skin to metal, super cold fuel and POL (petroleum, oil, lubricants), wind chill, and tight clothing, particularly boots.
- Riding in open vehicles, exposure to propeller/rotor-generated wind, running or skiing, and altitude exposure where there is little tree cover can all contribute to greater windchill.
Symptoms
- Numbness in affected area.
- Tingling, blistered, swollen, or tender areas.
- Pale, yellowish, waxy-looking skin (grayish in dark-skinned soldiers).
- Frozen tissue that feels wooden to the touch.
- Significant pain after rewarming
Prevention
- Monitoring air temperature and wind speed and using the windchill index is the only way to determine the relative risk of frostbite.
- Use contact gloves to handle all equipment; never use bare hands.
- Use approved gloves to handle all fuel and POL (petroleum, oil, lubricants) products.
- Avoid cotton clothing, which holds perspiration in cold-weather environments.
- Keep face and ears covered and dry.
- Keep socks clean and dry.
- Avoid tight socks and boots.
Treatment
- Immersion of the affected part in a warm (98-104°F) water is very effective, however most minor cases of frostbite can be re-warmed at room temperature or against a buddy’s skin.
- Once a tissue is thawed, it must not freeze again. If there is the possibility of tissue refreezing, it is better not to thaw it in order to avoid damaging tissue further.
- Avoid exposure to excessive heat (open flame, stove tops, steam, heat packs) or rubbing affected tissue.
- All Soldiers with a peripheral freezing injury must be suspected of being hypothermic and treated appropriately. During field management, it is more important to prevent hypothermia than to rewarm frostbite rapidly
Non-Freezing Cold Injuries
The most common non-freezing cold injuries are chilblain and trenchfoot. Trench foot occurs when tissues are exposed to temperatures from 32-60°F for prolonged periods of time (>12 hrs), whereas chilblains, which is a more superficial injury, can occur after just a few hours of exposure. A non-freezing cold injury is classified by the symptoms and stages of recovery.
Chilblain

Chilblain is a non-freezing CWI that can occur after 1-5 hours in cold-wet conditions when skin temperature is > 32°F/0°C. The most commonly affected areas are the dorsal surface of the fingers, but the ears, face, and other exposed skin are also areas of occurrence. There are no lasting effects from chilblains.
Cause
- Continuous or repeated exposure of skin to cold/wet weather conditions at temperatures below 50 °F for more than 1-5 hours.
Symptoms
- Chilblain lesions are swollen, tender, itchy and painful.
- With re-warming, the skin becomes swollen, red (or darkening of the skin in dark-skinned soldiers) and hot to the touch. An itching or burning sensation may continue for several hours after exposure.
- Early diagnosis of chilblains becomes evident when symptoms do not resolve with re-warming.
Prevention
- Use contact gloves to handle all equipment; never use bare hands.
- Use approved gloves to handle all fuel and POL (petroleum, oil, lubricants) products.
- In extreme cold environments, do not remove clothing immediately after heavy exertion (PT); wait until you are in a warmer location.
- Avoid cotton clothing, which holds perspiration, in cold-weather environments.
Treatment
- Re-warm affected area, keep warm and dry.
