Assessment & Management of Patient’s With Spinal Cord Injuries
Published .
The scene size up provides the first clue of a spinal cord injury. The mechanism of injury will lead the medics to provide manual stabilization of the cervical spine during the primary survey.
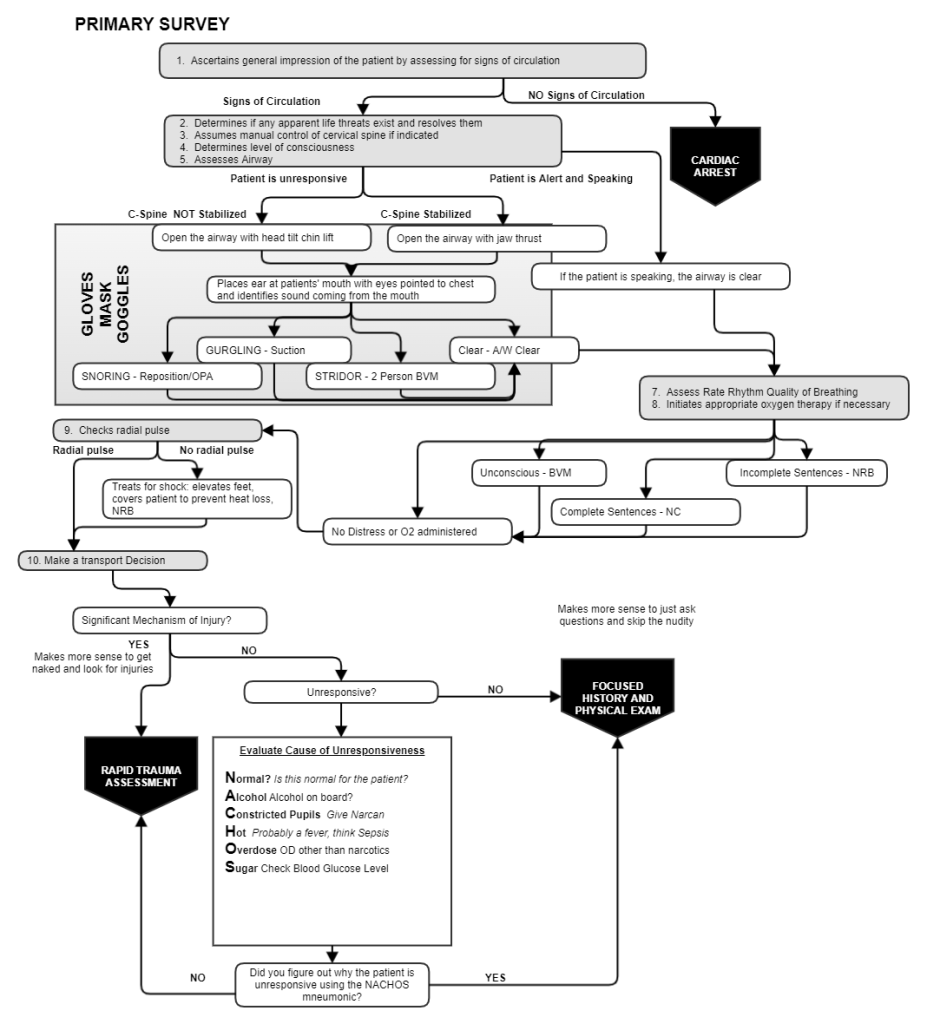
Initial management of the patient is always guided by the primary survey. Manually stabilizing the patient’s cervical spine is the third priority upon reaching the patient. The worst bone a person can break is their neck. Any movement of the spine could shift a vertebrae into the spinal cord resulting permanent paralysis or apnea.
At the point of the primary survey, the medics are not really in a position to definitively determine the presence of a spinal cord injury. The medics base their decision to manually stabilize the cervical spine on the mechanism of injury. The medics ensure the neck is maintained in a neutral and inline position through movement to the ambulance and during transport.
Manual stabilization also affects how the medics would open the airway in the event the patient is unresponsive. Opening the airway with the head-tilt-chin lift could result in further damage to the cervical vertebrae. Opening the airway with the jaw thrust will open the airway while the neck is maintained in a neutral and inline position.
If the patient is found in a seated position (like the drivers seat), the medics could move the patient from the car with a vest style extrication device. Such a device will make it easy to ensure manual stabilization of the cervical spine during movement from the vehicle and to the ambulance. There are 3 acceptable ways to move a patient with a potential spinal cord injury:
- Utilize a vest type device to immobilize prior to moving the patient from the vehicle. This measure provides the most amount of cervical protection during movement and also makes it easier to move the patient as such device have handles that can be used to pull the patient from the vehicle.
- Carefully rotate the patient from the vehicle using the rapid extrication technique. The technique does not provide the same level of protection from movement as the vest type device, but takes less time. It’s also more difficult to move the patient.
- An emergency move may be needed if the vehicle is unstable or on fire. This method provides the least amount of protection from movement and is only performed in dire situations.
Before the head is secured to a long back board or vest style immobilization device, a properly sized rigid cervical collar should be applied. After the patient’s torso is secured, the head can be immobilized to a device. This measure assumes the patient is going to vomit. If the patient vomits while the cervical spine is being immobilized, the patient can be log rolled while manual stabilization is still being performed. This measure will allow the medics to quickly clear the airway without compromising the patient’s cervical spine.
Patient’s with helmets may need them removed in order for the medics to control the airway. Helmets are always best left on the patient’s head, however the need to open and clear the airway may dictate it be removed. Medics should practice helmet removal techniques on a regular basis. If a patient is immobilized with the helmet on, the medics must pad under the shoulders the same way they would pad an infants shoulders if the infant was being immobilized.
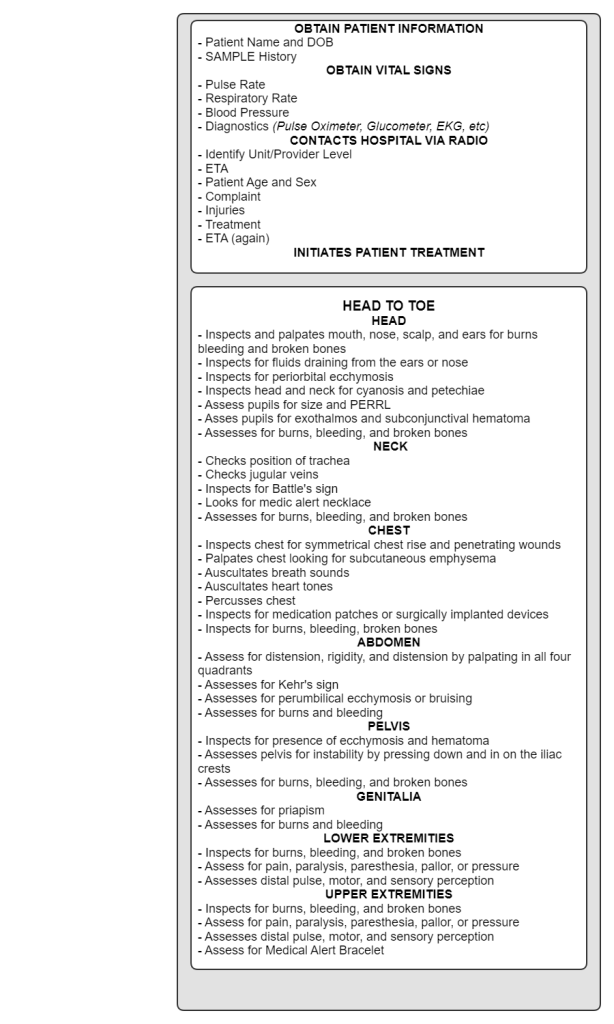
Actual evidence of a spinal cord injury should be found miles away from the scene in the back of the ambulance. Once in the back of the ambulance, the medics should perform a secondary survey. The secondary survey begins with vital signs and SAMPLE interview. During the head to toe exam that the medics would find absence in pulse, motor, or sensory perception (assuming the patient is conscious). Any deficits should be reported to the ED and documented.
