Assessment & Management Of Patients With Brain Injuries
Published (updated: ).
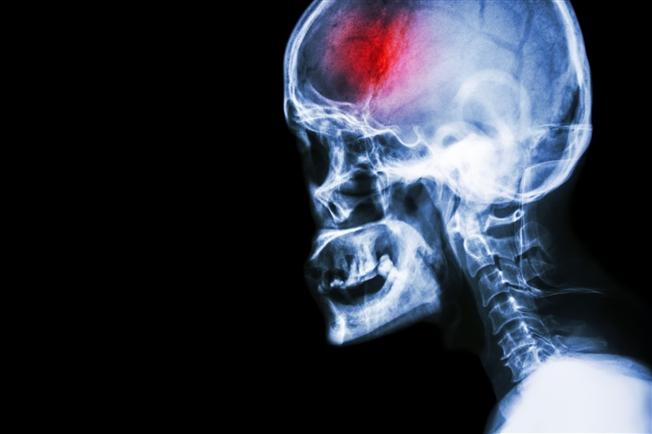
A head injury is a broad term that describes a faster rate of injuries that occur to the scalp, skull brain and underlying tissue and blood vessels in the head . Head injuries are commonly referred to as a brain injury or traumatic brain injury (TBI) depending upon the extent of the head trauma. Head injuries can result from a variety of mechanisms of injury. Blunt trauma seems to be the most common mechanism of injury however penetrating injury to the head Is well-represented. Like all injuries to bones, a head injury can be open or closed.
Head injuries can present with a variety of different symptoms depending upon the location and severity of the injury. The following signs and symptoms are most associated with head injuries:
- Cerebrospinal fluid – Cerebrospinal fluid (CSF) it suspected when clear drainage is seen from the ears or nose
- Discoloration around the eyes – This is seen typically during an inspection of the face during the secondary survey. A finding of discoloration around the eyes indicates blood draining around the orbits from a basilar skull fracture. This finding is often referred to as raccoon’s eyes.
- Discoloration around the ears – A finding of discoloration around the ears indicates blood draining from a basilar skull fracture. This finding is often referred to as Battle’s sign.
- Skull deformity – A deformity to the skull or finding of crepitus indicates a skull fracture.
- Decreased mentation – A finding of altered mental status associated with a head injury is typically suspected to be an axonal injury. There are three grades of axonal injuries, mild, moderate, and severe. These types of injuries are easy to differentiate with the help of the Glasgow Coma Scale. A mild diffuse axonal injury is referred to as a concussion as well as a traumatic brain injuries (TBI).
- Irregular breathing pattern – Irregular breathing patterns are typically the result of injury to the brain stem. either directly injured or indirectly affected by increased intracranial pressure, various abnormal respiratory patterns can be seen.
- Unequal pupils – Anisocoria or unequal pupils can be the result of a direct injury to the nerves of the eye or the pupils can be indirectly affected by increased intracranial pressure.
- Nausea and vomiting – Nausea and vomiting are the most common symptoms of a head injury.
- Seizure activity – Seizure activity can be the result of direct injury to the brain or indirectly affected by an increase in intracranial pressure.
- Elevated blood pressure – Elevated blood pressure is common for any type of injury or illness to the brain. When there is an obstruction to blood flow in the brain, the body will increase blood pressure with a goal of removing an obstruction such as a blood clot. this increase in blood pressure is reflexive and a useful sign for medics
- Slow heart rate – Typically the result of increased intracranial pressure, the reflexive increase in blood pressure will eventually result in a decrease in heart rate. the heart rate will increase in order to increase blood pressure. The increased blood pressure signals the carotid and aortic baroreceptors to activate the parasympathetic nervous system, causing the heart rate to decrease.
Assessment of patients with brain injuries
Initial management of the patient is always guided by the primary survey. Patient’s with severe head injuries will likely be unresponsive or minimally not alert and require attention to detail regarding the airway and breathing. Patients who are not alert could be verbally responsive, painfully responsive, or unresponsive. Interventions such as suctioning to clear the airway and positive pressure ventilation are common for patients with severe head injuries. Due to the mechanism of injury or the finding of altered mental status, spinal precautions should be taken prior to moving the patient to the ambulance. Patients wearing helmets may need them removed in order to manage airway and breathing. It is important that medics know how to open, assess and manage a patient’s airway while cervical spine precautions are being maintained. Manually stabilizing the cervical spine, then opening the airway with a jaw thrust, then ventilating with a bag valve mask cannot be performed by 1 rescuer but must be performed by 2. Opening the patient’s airway with a head tilt chin lift may result in worsening of a patient cervical spine fracture.
After the patient has been loaded in the ambulance the medics should consider calculating a Glasgow coma scale. A GCS greater than 13 suggest a mild head injury while a GCS between 8 and 12 suggest a moderate head injury. Severe head injuries are considered when the patient has a GCS of less than 8. The patient’s vital signs can also point to a head injury. Not all head injuries produce hypertension. The SAMPLE history will reveal clues about the patients level of consciousness Immediately after the injury occurred. improving oxygenation it’s always a goal for medics when treating a brain injury. The brain injury patient may breathe normally or display any number of alternate respiratory patterns. Typically head injuries result in a spike in blood pressure, a finding of hypotension or shock in a patient with a head injury is a dire finding. Assessment of the patient’s vital signs, pupils, and neurological exam should all be performed in the back of the ambulance while enroute to the hospital. Assessment of pupils can also be helpful in determining the nature of the brain injury. These assessments are components of the secondary survey. Any abnormal finding should be reported to the hospital via radio in order to ensure the patient has a proper reception upon arrival at the hospital. It is recommended that patients with potential brain injuries be positioned with her head elevated at a 30° angle from their body.
