Anisocoria
Published (updated: ).

Anisocoria is a term derived from two Greek words, “aniso-” meaning unequal, “kore” meaning pupil, and a Latin suffix “ia” meaning abnormal condition. Anisocoria is characterized by a difference in pupil sizes. This phenomenon results due to disturbances in the efferent pathway dynamics. It can be physiological as well as pathological, occurring due to numerous causes, ranging from benign to life-threatening.
Important etiologies of anisocoria include third nerve palsy, Adie pupil, pharmacologic mydriasis, pharmacologic miosis, traumatic mydriasis, physiologic anisocoria, and Horner syndrome.
The prevalence of physiologic anisocoria is generally considered to be around 10 to 20%, which does not seem to differ greatly around the world. Physiologic anisocoria does not seem to have a sex predilection nor occurs at a specific age. Physiologic anisocoria is probably the most common cause. The prevalence of other causes of anisocoria is associated with the prevalence of the underlying condition.
Pathophysiology
Distinct pathways control miosis and mydriasis (dilation of the pupil). The parasympathetic pathway causes miosis by activating the iris sphincter. These pathways arise within the brain stem and then extend along cranial nerve III to finally innervate the iris sphincter. This pathway is activated by the pupillary light reflex and accommodation.
As mentioned before, anisocoria can be broken down into three categories:
- An inhibition of constriction of the pupil on one side – the pathological pupil remains larger than the other pupil (pupil is dilated), and this difference is more pronounced in light conditions
- An inhibition of dilatation of the pupil on one side – the pathological pupil remains smaller than the other pupil (pupil is constricted), and this difference is more pronounced in dark conditions
- Difference pupil sizes that in which the difference remains the same in light and dark condition – the anisocoria is more likely to be physiologic with neither pupil having pathology
As with many medical conditions, the first approach should be to get a good history from the patient, family, friends, and medical records. Finding out the timing of the onset of anisocoria occurred is very helpful, as a longstanding anisocoria is much less likely to represent a dangerous medical condition. Looking at an old picture of the patient can help show that the anisocoria may be chronic. Next, a thorough history of the medications the patient takes needs to be made, especially eye drops that have been put in the patient’s eye. A history of a recent visit to an eye doctor is also very helpful since the anisocoria could be caused by eye drops given during the visit.
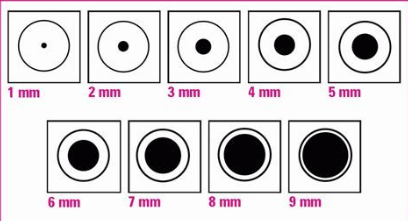
Once a thorough history has been taken, the abnormal pupil needs to be identified. To do this, both pupil sizes should be measured with the room lights on brightly and then again with the room lights dim. Having the room lights completely off may not be practical since the pupils need to be visible for measurement. To measure the pupil, a small ruler may be used. There are also near cards that have pupil sizes on them for comparison. While measuring the pupils, the patient should focus on a distant object. This is to avoid miosis (pupillary constriction) while the patient is accommodating at a near target. After the pupils have been measured, the practitioner should identify whether the anisocoria is greater in light or darker conditions.
Anisocoria greater in the light indicates the large pupil is the abnormal pupil due to poor pupillary constriction. Anisocoria greater in the dark indicates the small pupil to be abnormal due to poor pupillary dilation. A small amount of anisocoria that is equal in both light and dark conditions most likely represents physiologic anisocoria.
Other important aspects of the physical exam include assessing visual acuity at both distance and near. Worse near visual acuity in the eye with a larger pupil is more likely to indicate pharmacologic dilation from a cycloplegic medication. The swinging flashlight test should be performed to assess for a relative afferent pupillary defect.
