Assessment Of Soft Tissue Injuries
Published (updated: ).
Identifying the mechanism of injury in the scene size up is the first link to understanding the injury. Quite often, the mechanism of injury will not be significant enough to result in a cervical spine fracture but nonetheless results in a soft tissue injury. For instance, a patient could cut their arm in a rollover car accident or trip on a carpet and sustain a ground level fall. The injury is the same, but the process by which the medics approach the patient will differ due to the difference in mechanism of injury.
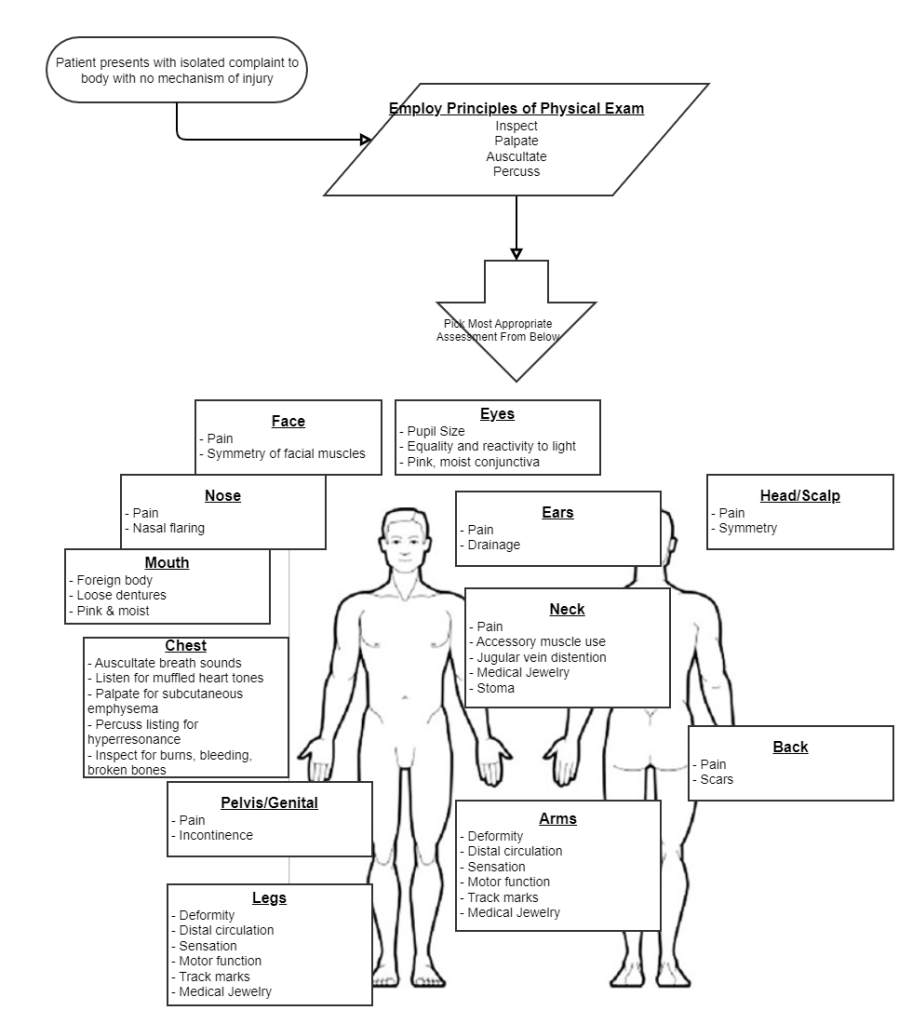
Initial management of the patient is guided by the primary survey. Once the primary survey has been completed, the medics need to perform a follow up assessment. If the mechanism of injury was significant, the medics will discover the injury when they look for injuries with the rapid trauma assessment. If the mechanism of injury was insignificant, the medics will discover the injury when they ask the patient, ‘why am I here?’ during the focused history and physical exam.
What If You Have To Ask Why Am I Here?
The SAMPLE survey guides the conversation between the medics and the patient. During this conversation, the medics can know what the patient’s complaints, medical history, and other helpful information. Obviously, a complaint that results in pain can be defined in terms of onset, provocation, quality, radiation, severity, and time.
The Rapid Trauma Assessment & Secondary Survey
Initial management of the patient is always guided by the primary survey. Once the patient’s needs for resuscitation have been addressed, the medics need to assess the abdomen. The medics may choose to look for injuries by performing the rapid trauma assessment.
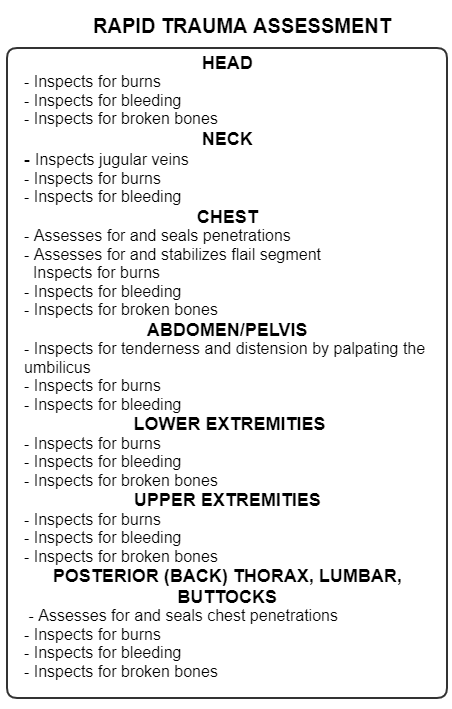
The rapid trauma assessment is performed anytime there is a significant mechanism of injury or the patient is unresponsive and the medics are unable to pinpoint the cause of the unresponsiveness. The rapid trauma assessment is intended to be performed while the patient is still on the scene. It is expected that medics will expose the patient and look for injuries. The purpose of the rapid trauma assessment is to look for time sensitive injuries that need to be addressed before the patient is even moved to the ambulance.
In the case of soft tissue injuries, at least on scene, the medics will be looking for burns, bleeding, and broken bones. It is important that the medics use all available hands to treat any injuries encountered. The very first intervention made by the medics will be identify bleeding and take measures to stop the bleeding (direct pressure).
Soft tissue injuries come in various presentations. Impaled objects should be stabilized with bleeding carefully controlled without manipulating the impaled object. Amputations can present significant bleeding (or very little bleeding). Once the bleeding is controlled, the amputated extremity should be located, placed in a plastic bag, and kept in ice with the intent of re-attachment at the hospital. Shootings can present with an entry wound and an exit wound that must be managed (preferably prior to movement into the ambulance). Avulsions are an injury that results in torn skin that has been pulled away from the body. Care should be taken to ensure avulsed skin remains intact and bandaged with the rest of the wound.
Bleeding is a primary concern when managing a soft tissue injury. Assuming bleeding has been controlled, the medics may need to worry about wound contamination. Many times dirt and and other contaminants can find their way into the wound. For this reason, ambulances typically carry irrigation fluid that can be poured onto a wound to flush the debris out of the wound cavity.
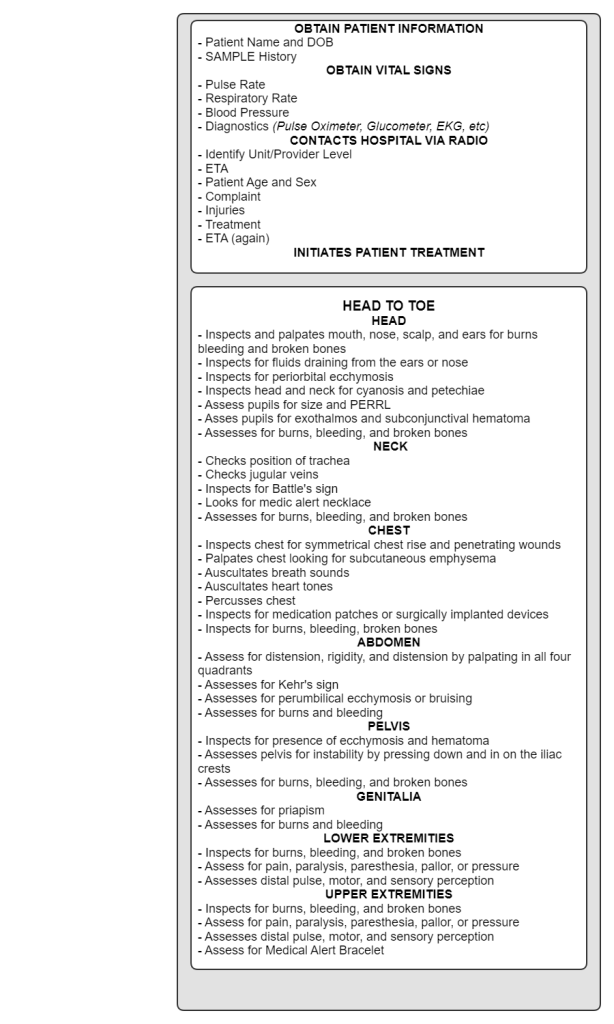
During the head to toe component of the secondary survey, the medics will look for burns bleeding, and broken bones. The reason these are checked in the ambulance and on scene is due to the possibility that the patient may not have assessed prior to movement. This is often the case in motor vehicle accidents where the patient is removed from the car on a long backboard. Nobody would choose to move an injured person first without looking for injuries, but in the case of a car accident, assessing the patient for injuries prior to movement is often impossible.
In addition to looking for burns, bleeding broken bones, the medics will assess pulse, motor, and sensory perception in all 4 extremities. The medics will assess the patient for pain, paralysis, pressure, pallor, or paresthesia to determine if compartment syndrome is present.
Complications of soft tissue injuries
Bleeding, either internal or external left unchecked can lead to shock. Shock is a condition of hypoperfusion or hypotension that can prolong a seriously injured patient’s life. Medics should recognize the presence or possibility of this condition when assessing patients due to the fact that the patient requires rapid medical intervention. Further, shock requires the medics treat the patient gently as abrupt movements can result in rapid decompensation.
Pain is a real consideration. Soft tissue injuries are painful. The EMS system should be able to provide advanced life support personnel to the scene to provide narcotics or other analgesics.
Infection is another concern. Patient’s with soft tissue injuries may survive the injury, but later die of infection. Open wounds can easily become infected as pathogens have a clear route into the patient’s body. Despite being closed off to the world, closed wounds also present the patient with an infection risk. Immunocompromised patients with soft tissue injuries are at a distinct disadvantage for infection. Keeping wounds covered with clean bandages can help mitigate the risk of infection for patients with soft tissue injuries.
