Assessment Of Orthopedic Injuries
Published (updated: ).
Identifying the mechanism of injury in the scene size up is the first link to understanding the injury. Quite often, the mechanism of injury will not be significant enough to result in a cervical spine fracture but nonetheless results in a long bone fracture or dislocation. For instance, a patient could break their arm in a rollover car accident or trip on a carpet and sustain a ground level fall. The injury is the same, but the process by which the medics approach the patient will differ due to the difference in mechanism of injury.
Initial management of the patient is guided by the primary survey. Once the primary survey has been completed, the medics need to perform a follow up assessment. If the mechanism of injury was significant, the medics will discover the injury when they look for injuries with the rapid trauma assessment. If the mechanism of injury was insignificant, the medics will discover the injury when they ask the patient, ‘why am I here?’ during the focused history and physical exam.
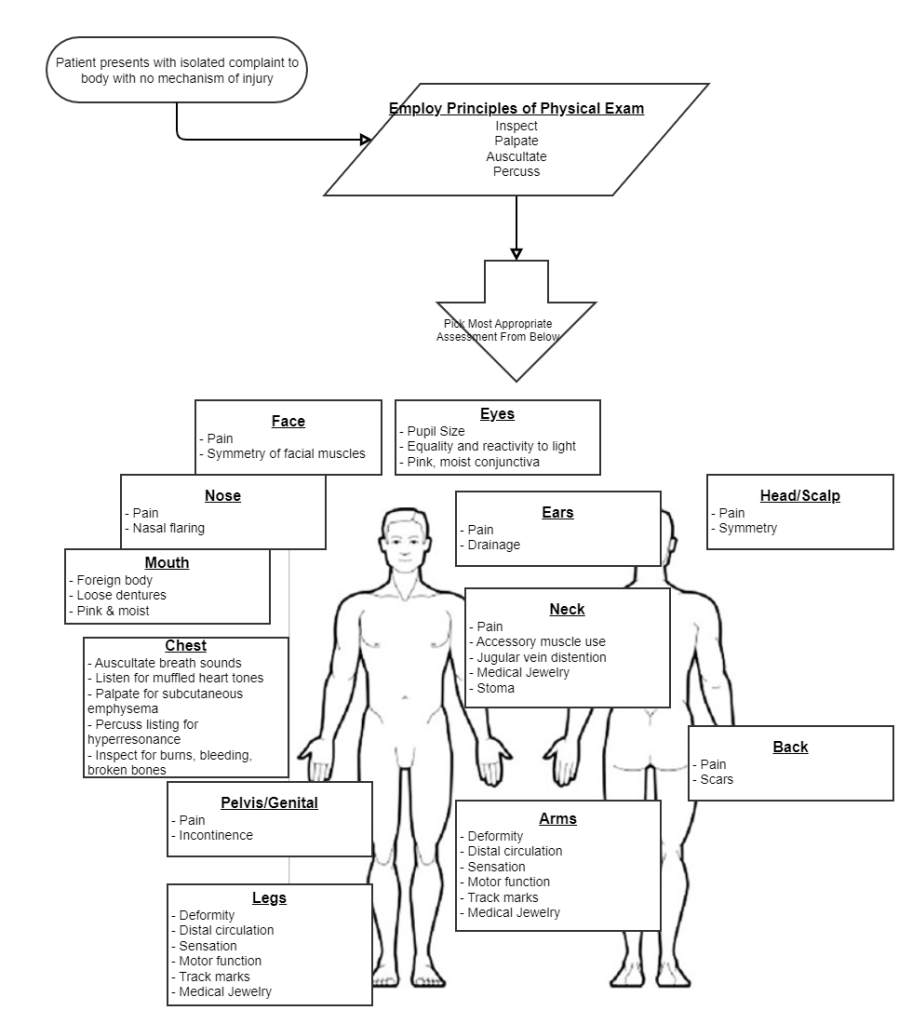
What If You Have To Ask Why Am I Here?
The SAMPLE survey guides the conversation between the medics and the patient. During this conversation, the medics can know what the patient’s complaints, medical history, and other helpful information. Obviously, a complaint that results in pain can be defined in terms of onset, provocation, quality, radiation, severity, and time. When it comes to an orthopedic complaint, additional details could be helpful to find an uncommon but impossible to find otherwise injury that sometimes results in amputation.
Acute Compartment Syndrome
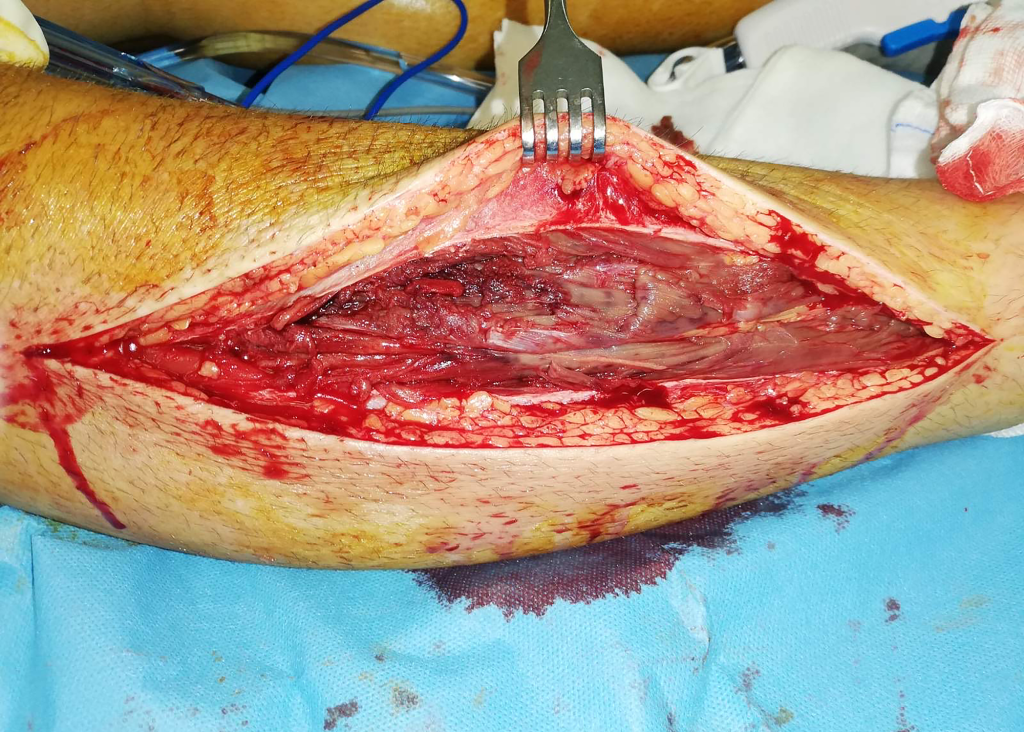
Acute compartment syndrome occurs when there is increased pressure within a closed osteofascial compartment, resulting in impaired local circulation. Acute compartment syndrome is considered a surgical emergency since, without proper treatment, it can lead to ischemia and eventually necrosis.
Fascia is a thin, inelastic sheet of connective tissue that surrounds muscle compartments and limits the capacity for rapid expansion. In the leg, there are four muscle compartments: anterior, lateral, deep posterior, and superficial posterior. The anterior compartment of the leg is the most common location for compartment syndrome. This compartment contains the extensor muscles of the toes, the tibialis anterior muscle, the deep peroneal nerve, and the tibial artery.
Other locations in which acute compartment syndrome is seen include the forearm, thigh, buttock, shoulder, hand, and foot. It can also be seen in the abdomen, but more commonly, it presents in the limbs. Significant attention should be paid to patients with open fractures. Recent retrospective studies indicate that skin laceration would not relieve the pressure inside the muscle compartments. Therefore, acute compartment syndrome is still predictable.
Acute compartment syndrome typically occurs within a few hours of inciting trauma. However, it can present up to 48 hours after. The earliest objective physical finding is the tense, or ”wood-like” feeling of the involved compartment. Pain is typically severe, out of proportion to the injury. Early on, pain may only be present with passive stretching. However, this symptom may be absent in advanced acute compartment syndrome. In the initial stages, pain may be characterized as a burning sensation or as a deep ache of the involved compartment. Paresthesia, hypoesthesia, or poorly localized deep muscular pain may also be present.
Classically, the presentation of acute compartment syndrome has been remembered by “The Five P’s”: pain, pulselessness, paresthesia, paralysis, and pallor.However, aside from paresthesia, which may occur earlier in the course of the condition, these are typically late findings. Beware that the presence or absence of a palpable arterial pulse may not accurately indicate relative tissue pressure or predict the risk for compartment syndrome. In some patients, a pulse is still present, even in a severely compromised extremity.
Physical exam should focus on the neurovascular territory of the involved compartment:
- Observe skin for lesions, swelling, or color change
- Palpate over the compartment, observing temperature, tension, tenderness
- Check pulses
- Evaluate two-point discrimination and sensation
- Evaluate motor function
Although the clinical features discussed above can help identify compartment syndrome, they have limited sensitivity and specificity. Other factors, such as compartment pressures, can help make the diagnosis. Due to the potential for rapid progression of compartment syndrome, clinicians should perform serial exams.
Obvious Signs of Injury
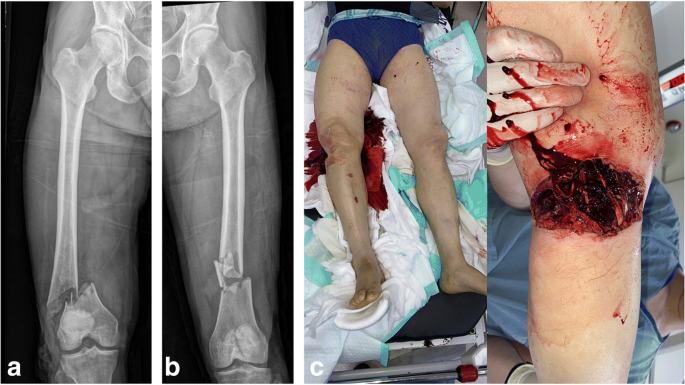
Unlike compartment syndrome, the vast majority of orthopedic injuries are obvious and require very little in discernment to determine their presence. External bleeding is an obvious sign that requires immediate attention, but what about internal bleeding? Internal bleeding associated with an orthopedic injury looks like swelling on the outside. The largest blood vessels in the body are attached to bones. Every long bone fracture will have some sort of vascular consequence.
The natural reaction of a patient with a broken bone will be to guard the area of the fracture. This patient will unknowingly stabilize the fracture even if they are unaware of it’s existence. Self stabilization plays into the medics agenda given all they have to do is splint since the patient is performing the duties of stabilization.
The Rapid Trauma Assessment & Secondary Survey
Initial management of the patient is always guided by the primary survey. Once the patient’s needs for resuscitation have been addressed, the medics need to assess the abdomen. The medics may choose to look for injuries by performing the rapid trauma assessment.
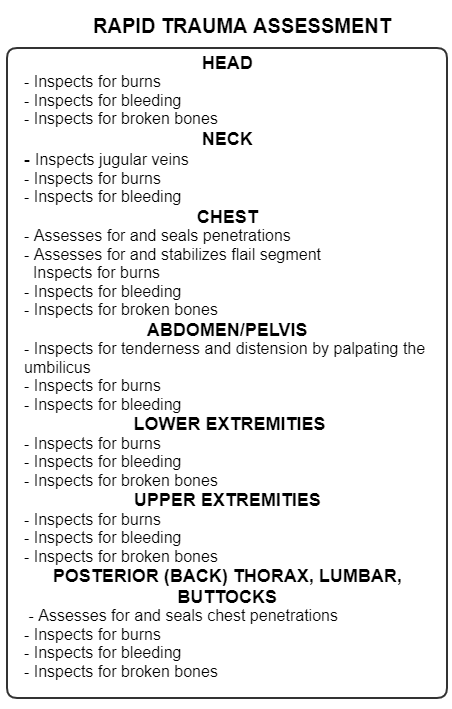
The rapid trauma assessment is performed anytime there is a significant mechanism of injury or the patient is unresponsive and the medics are unable to pinpoint the cause of the unresponsiveness. The rapid trauma assessment is intended to be performed while the patient is still on the scene. It is expected that medics will expose the patient and look for injuries. The purpose of the rapid trauma assessment is to look for time sensitive injuries that need to be addressed before the patient is even moved to the ambulance.
In the case of orthopedic trauma, at least on scene, the medics will be looking for burns, bleeding, and broken bones. It is important that the medics use all available hands to treat any injuries encountered. The very first intervention made by the medics will be to stabilize any broken bones, then plan to splint the extremities to a long backboard.
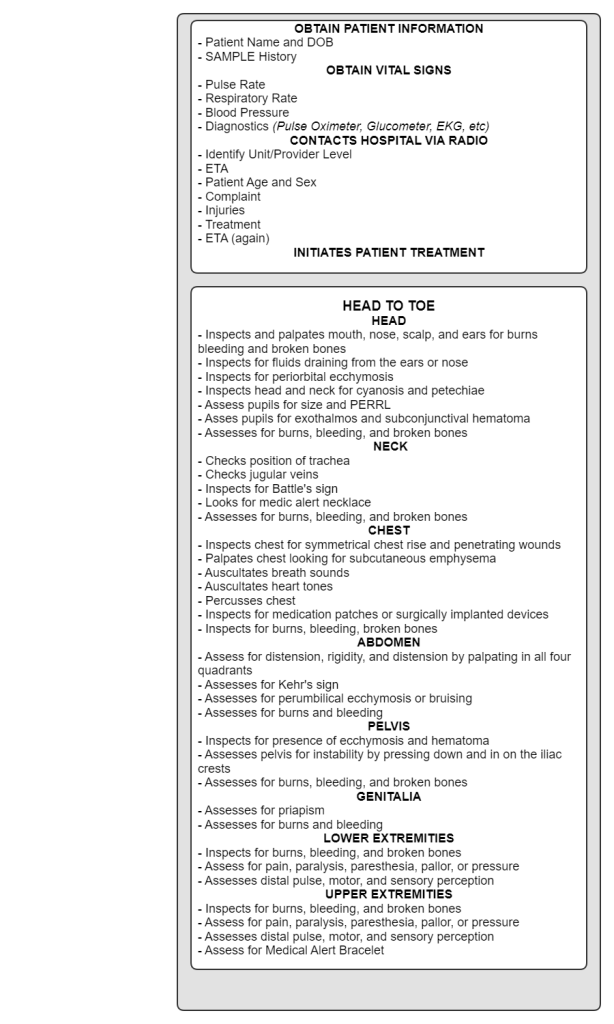
During the head to toe component of the secondary survey, the medics will look for burns bleeding, and broken bones. The reason these are checked in the ambulance and on scene is due to the possibility that the patient may not have assessed prior to movement. This is often the case in motor vehicle accidents where the patient is removed from the car on a long backboard. Nobody would choose to move an injured person first without looking for injuries, but in the case of a car accident, assessing the patient for injuries prior to movement is often impossible.
In addition to looking for burns, bleeding broken bones, the medics will assess pulse, motor, and sensory perception in all 4 extremities. The medics will assess the patient for pain, paralysis, pressure, pallor, or paresthesia to determine if compartment syndrome is present.
