Complications of Fractures
Published .
Hemorrhage
Pelvic, hip and long bones are highly vascular and fracture can result in significant bleeding. Blood loss from a closed femoral fracture is estimated to be between 1000 mL and 1500 mL, and for closed tibial fractures 500 mL and 1000 mL. For open fractures, when the skin is breached, these figures may double. Surgical fixation techniques include plate and screws, intramedullary nailing (a rod placed down the middle of the bone) or a form of joint replacement. Determining which technique to use depends on the location of the injury, type of fracture and functional requirements of the person. Surgical fixation of pelvic, hip and long bones often results in a large amount of blood loss and this is combined with loss from the initial injury.
Instability
Over 6,300,000 people in the United States sustain fractures each year. The current trend in treating adult diaphyseal long bone fractures is to surgically stabilize them early after injury, in order to more rapidly mobilize patients. However, an increased “healing rate” has been observed in patients treated with delayed fixation, suggesting that there may be benefits in waiting to stabilize fractures. These biological benefits include the stimulation of callus formation, the improvement of mechanical properties of the callus, and a decreased rate of non-union. Although it has been proposed that delaying fixation may boost inflammatory response and provide extra stimulation to cells that are responsible for fracture healing, the exact mechanisms underlying fracture repair stimulation remain largely unknown. Whether delayed stabilization can affect stem cell differentiation and alter the mode of fracture healing has not been well determined.
Loss of Tissue & Blood Supply
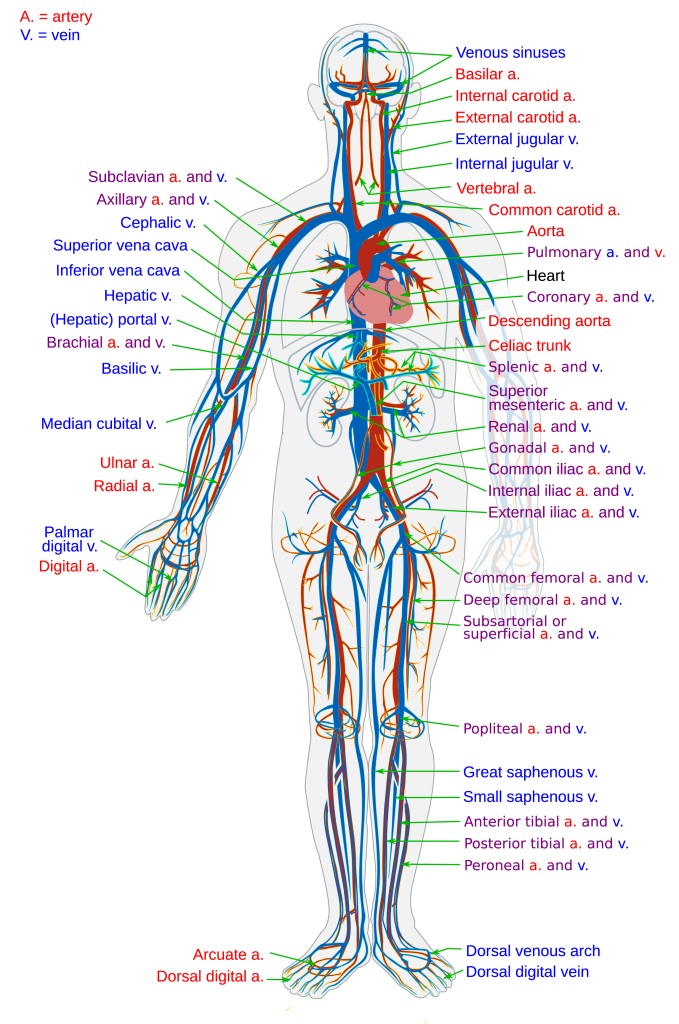
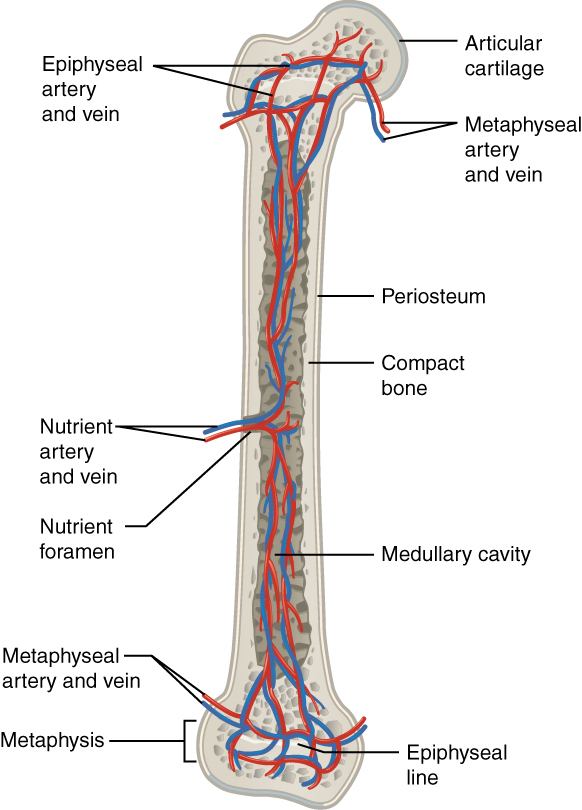
All biological tissues, including bone, require vascular support to survive. However, a frequently overlooked feature of bone is its extensive vascular network. Many studies have demonstrated that the blood vessels in bone are necessary for nearly all skeletal functions, including development, homeostasis, and repair. In addition, blood vessels lost due to trauma are regenerated, and new bone tissue formed in response to injury is vascularized. As a consequence of this environment, the blood vessels in bone are highly active, not simply a passive source for the delivery of nutrients.
The rate at which blood vessels deliver oxygen, nutrients, growth factors, and circulating cells to boneis tightly regulated as a function of blood pressure and vascularization. Given that blood pressure is generally maintained, the number and size of blood vessels determines the local blood flow rate. These two factors are regulated through the processes of angiogenesis and vasomotor function, respectively.
The bones of the human body are made up of living cells that need a blood supply to stay healthy. In osteonecrosis, blood flow to part of a bone is disrupted. This results in death of bone tissue, and the bone can eventually break down and the joint will collapse. Osteonecrosis is also called:
- Avascular necrosis.
- Aseptic necrosis.
- Ischemic necrosis of bone.
Osteonecrosis can happen to any bone, but most often it develops in the ends of long bones, such as the:
- Thigh bone (femur), especially the upper part—the ball in the hip socket. The lower end, which is part of the knee joint, is also often affected.
- Upper arm bone (humerus), especially the upper part—the ball in the shoulder joint.
When the disease involves part of a bone in a joint, it can lead to the breakdown of the bone and arthritis. Less often, the bones of the elbows, ankles, feet, wrists and hands are affected. The primary symptom of osteonecrosis is pain, and doctors usually diagnose the disease using imaging methods such as x-rays or magnetic resonance imaging (MRI). Most people require surgical treatment to prevent further bone damage, to protect the bones and joints, and to improve use of the joints. Doctors have identified a number of risk factors that may make a person more likely to get osteonecrosis. However, some people who get the disease do not have any known risk factors. The risk factors may include a broken or dislocated bone or a joint injury may damage the surrounding blood vessels. This can decrease the blood supply to the bone and lead to osteonecrosis.
Contamination
The majority of fractures (broken bones) do not lead to infections. When infections do occur after fractures, the treatment and recovery can be prolonged and complicated.
Infections typically occur in fractures because bacteria enter the body during the traumatic event. Although uncommon, bacteria can also enter the body during surgery to set the broken bones.
If the bone breaks in such a way that bone fragments stick out through the skin or a wound penetrates down to the broken bone, the fracture is called an “open” or compound fracture. The skin is normally a barrier to outside contaminants, including bacteria. However, when the skin is broken, bacteria can easily travel down to the broken bone and possibly cause an infection.
During surgery to fix a fracture, the skin and soft tissues are cut in order to reach the broken bone. The risk for developing an infection in this setting is quite low, usually less than 1% in healthy individuals. Preventative antibiotics are given to patients prior to surgery and high standard of care in Operating Theater help prevent infection.
In general, the greater the damage is to the surrounding skin, muscles, arteries, and veins near the fracture site, the higher the risk for infection.
Chronic diseases that lower your immune system may put you at greater risk for infection after fracture. Examples of these include:
- Diabetes mellitus
- HIV
- Rheumatoid arthritis
Long Term Disability
One major long-term impact of a broken bone is damage to the nerves. When a bone breaks, the nerves can be stretched, crushed and bruised. These secondary injuries are generally the result of blunt force trauma. A damaged nerve generally heals on its own, but the healing process can take months or even years depending on the degree of damage done. In some cases, a damaged nerve may never completely heal, causing a lifelong impact. This type of damage typically results from a sharp bone fragment contacting the nerves after a break.
Another common long-term impact of a bone fracture is decreased strength around the site of a fracture and increased discomfort. For instance, if you break your forearm, you may find this area is not as strong as it once was and you cannot move it as you once could.
Although fractures damage the bone, it can also impact the surrounding muscles, joints and ligaments. Fractures can damage the cartilage at the ends of the bone, known as the joint or joint surfaces. When the cartilage is damaged, the smooth surface scars, which can ultimately result in osteoarthritis. This can cause stiffness in your joints and a limited range of motion.
Serious bone fractures can also result in serious psychological trauma as well. Depending on how bad the break was and how it has impacted your life, you may experience a range of psychological conditions, such as depression, anxiety and stress.
If a fracture does not heal properly, it can hold you back from certain daily activities. What once was a simple task for you, could now become a challenge or roadblock.
Pregnancy With Pelvic Fracture
Pelvic fractures in pregnant women are usually high-energy injuries associated with risk of mortality to both mother and fetus. The mother’s life always takes priority in the acute setting as it offers the best chance of survival to both the mother and the fetus. Indications for operative intervention of acute pubic symphysis rupture depend on presence of an open disruption, amount of displacement, and degree of disability
