Assessment & Management Of Abdominal Trauma
Published (updated: ).
Initial management of the patient is always guided by the primary survey. Once the patient’s needs for resuscitation have been addressed, the medics need to assess the abdomen. The medics may choose to look for injuries by performing the rapid trauma assessment.
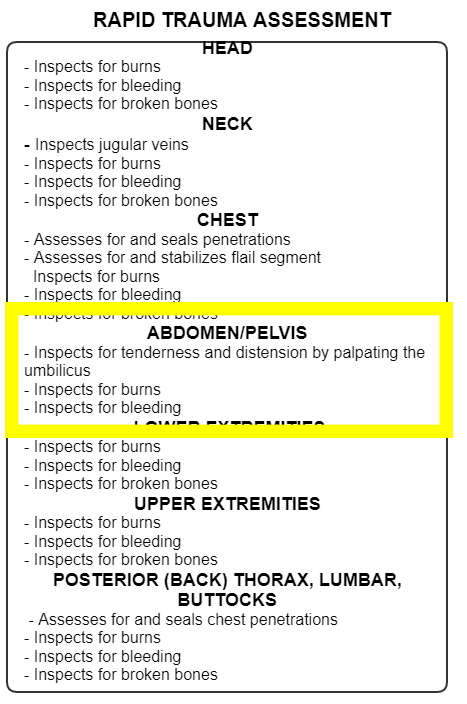
The rapid trauma assessment is performed anytime there is a significant mechanism of injury or the patient is unresponsive and the medics are unable to pinpoint the cause of the unresponsiveness. The rapid trauma assessment is intended to be performed while the patient is still on the scene. It is expected that medics will expose the patient and look for injuries. The purpose of the rapid trauma assessment is to look for specific injuries that need to be addressed before the patient is even moved to the ambulance.
In the case of abdominal trauma, the medics should look for bleeding. If encountered, the medics should apply direct pressure to control bleeding. Controlling bleeding with direct pressure will often be the only option for controlling bleeding to the abdomen. The medics will also look for abdominal distension or rigidity as a way to assess for internal abdominal bleeding.
Once the patient has been moved to the ambulance, the ambulance should quickly depart the scene. While enroute to the hospital , there is more work to be done. The medics obtain the patient’s name and date of birth, perform a SAMPLE survey, obtain vital signs, contact the hospital, and perform any care deferred for transport.
From the SAMPLE history, the medics should understand where the patient is hurting. A good question to ask any patient with abdominal pain be it medical or trauma is, “where does it hurt?” Getting an idea of where the injury is located can provide clues as to the affected organs. Left upper quadrant could mean spleen or stomach. Right upper quadrant could mean liver. Injuries to the hollow organs (like stomach, gallbladder, intestines) tend to be more painful immediately following the injury. Injuries to solid organs (liver, pancreas, spleen and adrenal glands) tend to take a little time to cause pain, Bleeding is much more significant in injuries to solid organs given the fact that they are very vascular.
Assessment of vital signs will provide the medics with valuable clues of the presence of an abdominal injury:
- Signs of shock – Hypotension, tachypnea, and tachycardia are classic signs of shock. Identifying and treating the patient who is experiencing shock will help the medics express the seriousness of the patient’s injury to the hospital.
- Tachypnea or shortness of breath – Most patients with an abdominal injury will experience some level of dyspnea. The dyspnea may be the result of an additional chest injury or could be caused by the pain that breathing with an abdominal injury can cause. Treating shortness of breath with oxygen should be reflexive and probably initiated prior to moving the patient to the ambulance. Pulse oximetry can be used to detect latent (hidden) hypoxia. A pulse oximetry reading above 94% could be a confirmation that that patient is breathing normally.
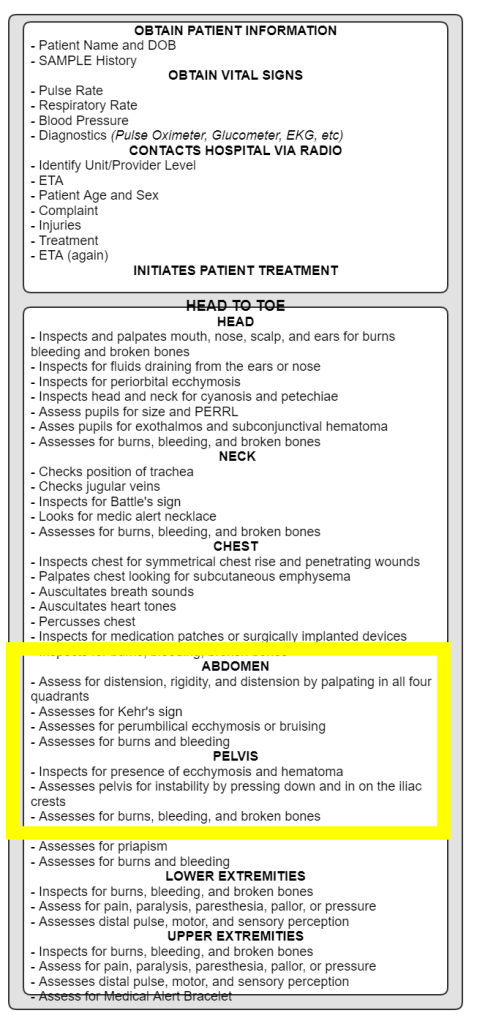
Next, the medics perform a comprehensive head to toe assessment. Sometimes, the medics will not be able to take a look at the patient’s injuries prior to moving the patients, therefore all of the observations that would have been made during the rapid trauma assessment are included in the head to toe assessment of the secondary survey. The abdomen should be assessed for the following:
- Distension or rigidity
- Palpation in all 4 abdominal quadrants – Assess each area looking for tenderness (obviously if the patient is conscious). The location of the tenderness often means the injury is laying just underneath the medics fingertips.
- Kehr’s Sign – the occurrence of acute pain in the tip of the shoulder due to the presence of blood or other irritants in the peritoneal cavity when a person is lying down and the legs are elevated. Kehr’s sign in the left shoulder is considered a classic symptom of a ruptured spleen.
- Periumbilical Ecchymosis – superficial edema with bruising in the subcutaneous fatty tissue around the peri-umbilical region. This finding suggests internal injury from blunt force trauma or hemorrhagic pancreatitis.
- Burns or bleeding
- Assessing the pelvis for stability – A pelvic fracture is a particularly dangerous fracture in that the pelvis is lined with blood vessels. When the pelvis is fractured and becomes unstable, movement of the patient could result in serious pain or internal bleeding.
Vaginal Bleeding
Vaginal bleeding can result from penetrating or blunt trauma. Adding to the concern of exsanguination is the possibility that the patient could be pregnant (where the medics are technically managing 2 patients). To stop vaginal bleeding, the medics (or patient) can apply direct pressure with a sterile absorbent vaginal pad. The medics should not insert their fingers into the vagina.
As much as possible, the medics should make an effort to protect the patient’s privacy and assure confidentiality. If the trauma is the result of a criminal act such as rape, the medics should avoid destroying the patient’s clothing to protect evidence. If possible, place the clothing in a paper bag to prevent degradation of evidence.
