Assessment Of Chest Injuries
Published (updated: ).
Collect Dots With The Rapid Trauma Assessment and Secondary Survey
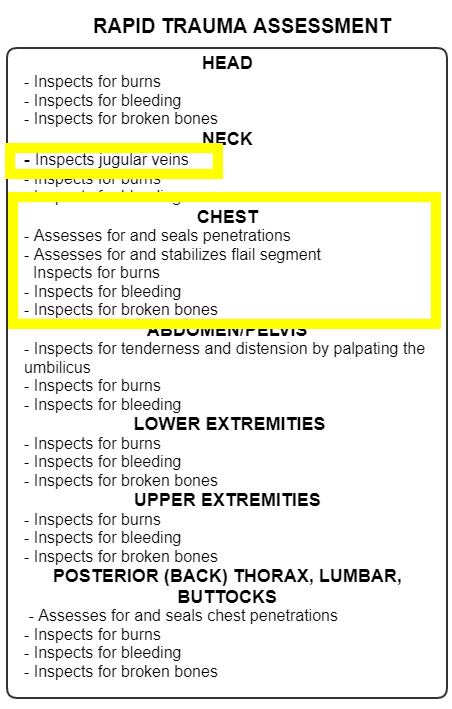
The rapid trauma assessment is performed anytime there is a significant mechanism of injury or the patient is unresponsive and the medics are unable to pinpoint the cause of the unresponsiveness. The rapid trauma assessment is intended to be performed while the patient is still on the scene. The purpose of the rapid trauma assessment is to look for time sensitive injuries that need to be addressed before the patient is even moved to the ambulance.

When looking for chest injuries, the medics should first note the presence of jugular vein distension. Jugular vein distension should tell the medics that there is a chest injury ahead. This reliable clue is seen when the medics are assessing the neck.
- Penetrating wound – Seal with an occlusive dressing
- Flail segment – Assistive ventilations will improve ventilation and will in some ways provide stabilization to the flail chest.
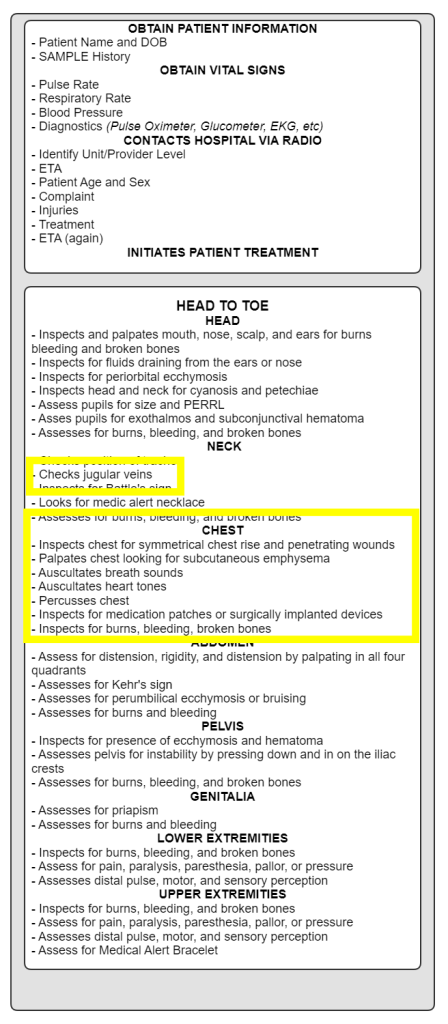
Once the patient has been moved to the ambulance, the ambulance should quickly depart the scene. While enroute to the hospital , there is more work to be done. The medics obtain the patient’s name and date of birth, perform a SAMPLE survey, obtain vital signs, contact the hospital, and perform any care deferred for transport. Next, the medics perform a comprehensive head to toe assessment. Sometimes, the medics will not be able to take a look at the patient’s injuries prior to moving the patients, therefore all of the observations that would have been made during the rapid trauma assessment are included in the head to toe assessment of the secondary survey.
Assessment of vital signs will provide the medics with valuable clues of the presence of a chest injury:
- Signs of shock – The main difference between a pneumothorax and a tension pneumothorax is shock. The shock is not caused from blood loss, but from obstruction of blood flow to the heart. The vena cava is sandwiched in the thoracic cavity between the lungs. The pressure changes in the chest associated with breathing create a vacuum that draws blood back to the heart. When there are large pockets of air inside the chest (but not in the lungs), the pressure is increased and the difference in pressure is not as pronounced. This leads to decreased venous return to the heart, resulting in decreased cardiac output.
- Irregular pulse or inconsistent radial pulse – Conditions that result in blood or fluids collecting in the pericardium (the sac that holds the heart) will result in a finding of pulsus paradoxus. Pulsus paradoxus is measured as a difference in blood pressure greater than 10mmHg associated with inhalation and exhalation. This measurement is difficult to assess in the ambulance, but medics could appreciate such a finding when assessing a radial pulse that seems to become stronger or weaker. In addition to an inconsistent pulse, the medics may also see an irregular heart rate associated with the changes.
- Tachypnea or shortness of breath – Most patients with a chest injury will experience some level of dyspnea. Treating shortness of breath with oxygen should be reflexive and probably initiated prior to moving the patient to the ambulance. Pulse oximetry can be used to detect latent (hidden) hypoxia. A pulse oximetry reading above 94% could be a confirmation that that patient is breathing normally.

The first clue of the presence of a chest injury is jugular vein distension. Jugular vein distension should tell the medics that there is a chest injury ahead. This reliable clue is seen when the medics are assessing the neck. Obvious injuries that should have been found during the rapid trauma assessment are:
- Penetrating wound – Seal with an occlusive dressing
- Flail segment – Assistive ventilations will improve ventilation and will in some ways provide stabilization to the flail chest.
Since the patient is already loaded in the ambulance and enroute to the hospital, the medics can look for other signs of a chest injury.
- Inspection of the chest – The medics should inspect the chest looking for asymmetrical chest rise which would indicate a flail chest. Another finding is unequal chest rise. Unequal chest rise would be seen as symmetrical chest rise, however one side of the chest appears to give more rise than the other. This finding suggests pneumothorax.
- Auscultation of breath sounds – Listening to see if one side of the chest has diminished breath sounds should raise the index of suspicion towards a pneumothorax
- Auscultation of heart tones – Listening to heart tones with a stethoscope may reveal muffled heart tones. Heart tones should sound crisp and clear, however if the heart tones are muffled should raise the index of suspicion towards pericardial tamponade. Pericardial tamponade is a life threatening condition that is best identified by EMS but treated by a physician at the emergency department.
- Palpation of the anterior chest wall – Palpation of the anterior chest could reveal the presence of pneumothorax. For the most part, a pneumothorax is obvious (the first clue being a penetration wound to the chest), however, some pneumothoraces are closed, and therefore not as obvious. While palpating the chest, the patient may complain of pain upon palpation (tenderness, obviously only a conscious patient could present with a finding of tenderness) may lead to clues of the presence of a chest injury. A sternal fracture can pretty much only be assessed by finding tenderness to the sternum.
- Percussion of the chest – Tapping on the chest could reveal areas of hyperresonance (An increased level of resonance or higher pitched sound than expected) or hyporesonance (A decreased level of resonance or lower pitched sound than expected).
The medics should also assess and treat any burns, bleeding, and broken bones. Assessing for implanted medical devices and medical patches rounds out the secondary survey.
