How People Die: Chest Trauma
Published .
Impaired Cardiac Output
.
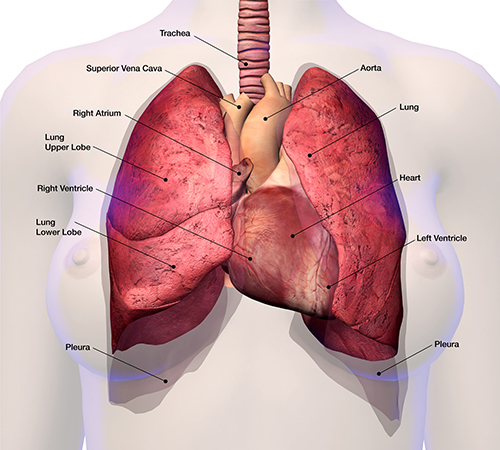
As a general rule, chest trauma of any sort increases the pressure in the thoracic cavity. This is evident by the typical finding of jugular vein distention. The jugular veins empty into the vena cava, but when the pressure in the chest is higher than normal it applies pressure to the vena cava. Increased pressure in the vena cava means decreased emptying of the jugular veins. Looking into the chest, the vena cava is nestled between the two lungs and aorta. The location of the vena cava and it’s tendency to be affected by pressure changes in the chest (primarily through inspiration and exhalation) leads to a vacuum that pulls blood from the body. A chest injury will result in increased pressure for longer than normal durations, resulting in less blood flow into the right ventricle. Decreased blood volume arriving at the right ventricle leads to decreased blood flowing out of the left ventricle. The increased pressure in the thoracic cavity decreases venous return to the heart, and ultimately decreases the amount of cardiac output.
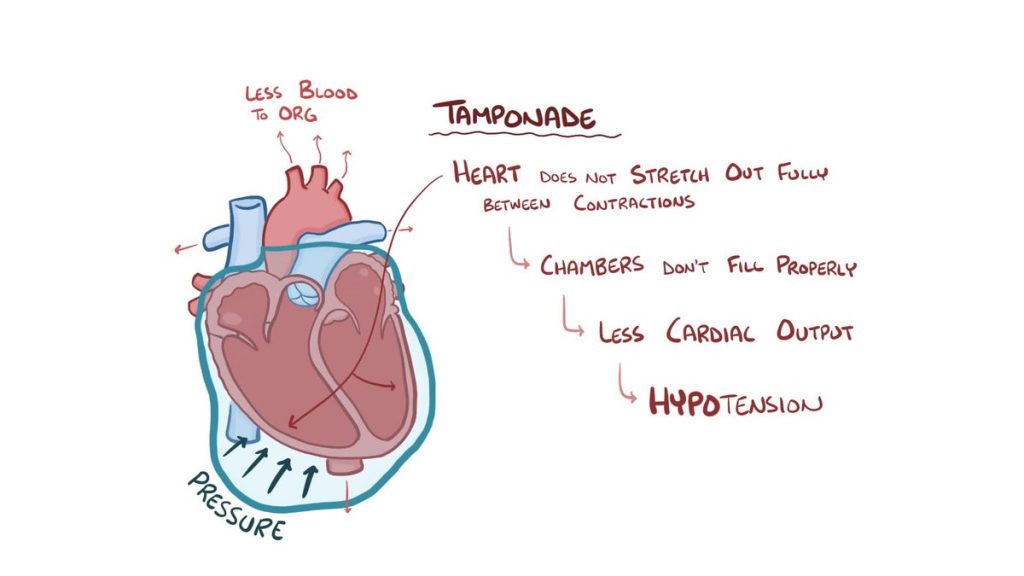
Another way the cardiac output can be decreased from a chest injury is if the heart is injured. A classic blunt force injury to the heart is pericardial tamponade. In pericardial tamponade, the pericardial sac (a sac that contains the heart) or one of the layers of the pericardium (pericardial sac) is injured and bleeding. If the bleeding is fast enough, it can fill the pericardium with blood, reducing the space in the pericardial sac. This decreased space in the pericardial sac will inhibit the normal stretching that ventricles do when filling with blood. Without the stretching, less blood will be pumped out of the heart leading to decreased cardiac output.
Impaired Ventilation
When a lung is leaking, the excess air will take the path of least resistance. In the case of a sucking chest wound, most of the air will exit the penetrating wound, but some of the air will remain in the chest but not necessarily in the lungs. There is only so much space in the thoracic cavity, so the collected air will fill the area typically used by the expanding lung for breathing. The result will be less air flow into the lungs. Less air flow will result in less exchange of oxygen can carbon dioxide.
Rib fractures can decrease the amount of air flowing in the lungs due to the lack of integrity of the rib cage. The lungs require intact ribs that can expand and contract as they were designed. When the patient has broken ribs, the structure that actually causes the lungs to expand is compromised, resulting in ventilation.
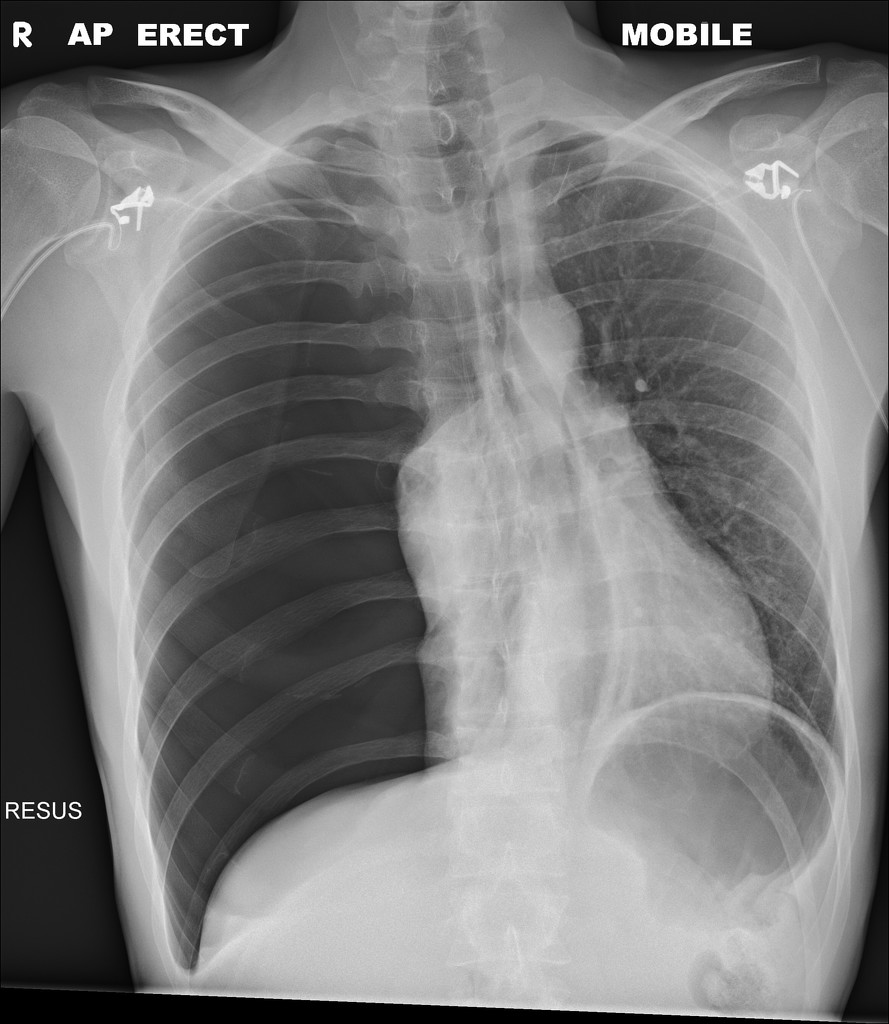
A collapsed lung (pneumothorax) is a buildup of air in the space between the lung and the chest wall. As more air builds up in this space, the pressure against the lung makes the lung collapse. This causes shortness of breath and chest pain because the lung cannot fully expand.
A collapsed lung is usually caused by an injury to the chest, but it may also occur suddenly without an injury because of a lung illness, such as emphysema or lung fibrosis. Your lung may collapse after lung surgery or another medical procedure. Sometimes it happens for no known reason in an otherwise healthy person (spontaneous pneumothorax).
Impaired Gas Exchange
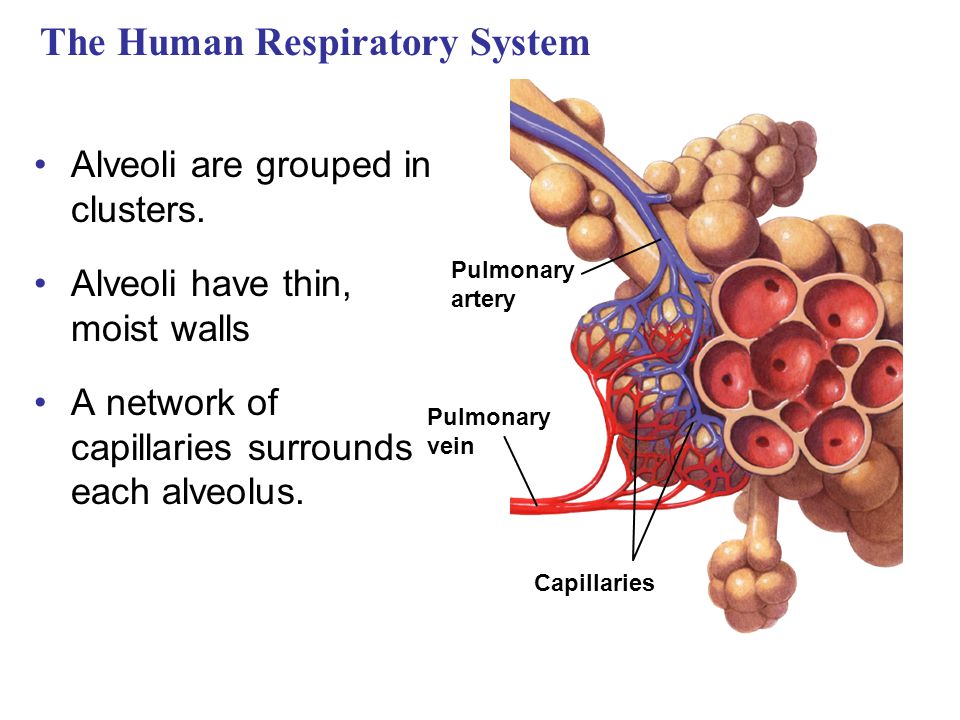
Normally, oxygen is brought into the lungs by breathing atmospheric air. The oxygen concentration in the atmosphere is 21% and the oxygen concentration in the red blood cells in the pulmonary capillaries is 16%. The capillaries are so thin that oxygen molecules can pass through the blood vessel wall. As the oxygen passes through the blood vessel walls, carbon dioxide is being released through the same blood vessel wall. The force that makes it all happen is diffusion. Less oxygen in the blood attracts oxygen from the environment. Less carbon dioxide in the environment means the blood will release the carbon dioxide into the environment.
Trauma to the chest often damages the tiny network of alveoli and pulmonary capillaries inside the lung. Any amount of force could cause one of the these alveoli to collapse (atelectasis). If these tiny blood vessels were to bleed, the blood would cover the alveoli and result in less gas exchange of carbon dioxide. An increase in air pressure in the lungs or thoracic cavity would affect the process of diffusion, leading to poor gas exchange.
Lung contusion is caused by blunt chest trauma, explosion injuries or a shock wave associated with penetrating trauma. These injuries damage alveolar capillaries, so blood and other fluids accumulate in the lung tissue, but it does not involve a cut or a tear of the lung tissue. The excess fluid interferes with gas exchange leading to hypoxia.
