Chest Trauma
Published .
Introduction
Thoracic trauma accounts for up to 35% of trauma-related deaths in the United States and encompasses a broad range of injuries that can cause significant morbidity and mortality. Prompt evaluation during the primary trauma survey is key to identifying those injuries that are immediately life-threatening and require rapid intervention.
Thoracic trauma is broadly categorized by mechanism into blunt or penetrating trauma. The most common cause of blunt chest trauma is motor vehicle collisions (MVC) which account for up to 80% of injuries. Other causes include falls, vehicles striking pedestrians, acts of violence, and blast injuries. The majority of penetrating trauma is due to gunshots and stabbings, which together account for 20% of all major trauma in the United States.
Blunt chest trauma is more common than penetrating trauma and directly comprises 20 to 25% of trauma deaths. Among patients presenting after motor vehicle collisions, higher morbidity and mortality are associated with high-speed collisions and with a lack of seat belt use. Despite its higher incidence, less than 10% of patients suffering blunt trauma to the thorax require operative intervention, whereas 15 to 30% of patients sustaining penetrating chest injuries will need operative intervention. Penetrating chest trauma is associated with higher overall mortality. Incidence varies based on geographic location, predominating in urban areas, those prone to interpersonal violence, and areas of conflict.
Anatomic Considerations and Pathophysiology
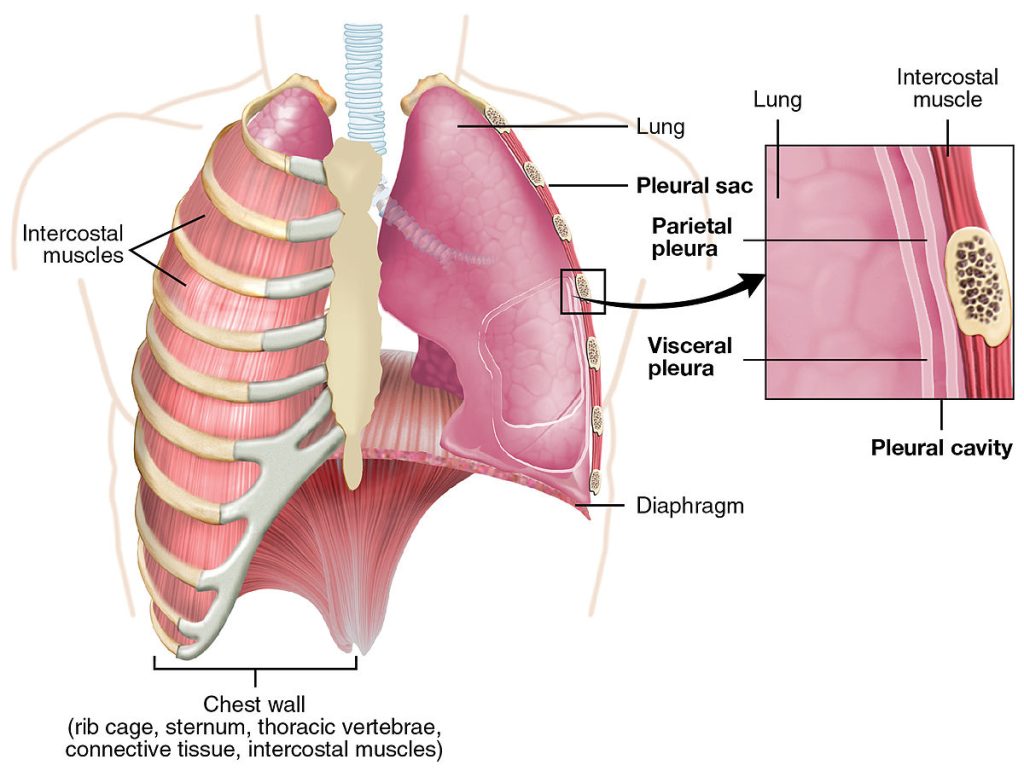
The major components of the chest wall are the rib cage, costal cartilage, and intercostal musculature. The blood supply and innervation to the chest wall are supplied by neurovascular bundles, comprising an intercostal artery, vein, and nerve that course at the inferior border of each rib. Deep to the rib cage, the parietal pleura makes up the inner lining of the chest wall. It receives somatic innervation from the intercostal nerves and therefore contains pain fibers. A layer of visceral pleura covers the intrathoracic structures. The potential space between the visceral and parietal layers is termed the pleural space and normally contains a small volume of hypotonic fluid, approximately 0.3 mL/kg, which undergoes constant turnover at a rate of 0.15 mL/kg per hour. This pleural fluid is produced by the parietal pleura itself and reabsorbed by pleural lymphatics. When lymphatic reabsorption is overwhelmed, pleural effusion occurs.
The chest wall serves 2 main purposes. First, it functions to facilitate respiration. Contraction of the diaphragm and intercostal muscles during inspiration increases intrathoracic volume, thus decreasing intrathoracic pressure, allowing the passive flow of air into the lungs. The reverse occurs during expiration. The diaphragm and intercostals return to their relaxed positions resulting in an increase in intrathoracic pressure, which forces air out of the lungs. The chest wall also protects intrathoracic structures from external injury. The sternum and clavicles provide additional structural support to the anterior thorax. They are dense bones that serve as points of attachment for the pectoralis major and minor muscles and therefore require significant force to fracture. Similarly, the scapulas which overlie the superior aspect of the posterior chest wall provide an added protective barrier to trauma.
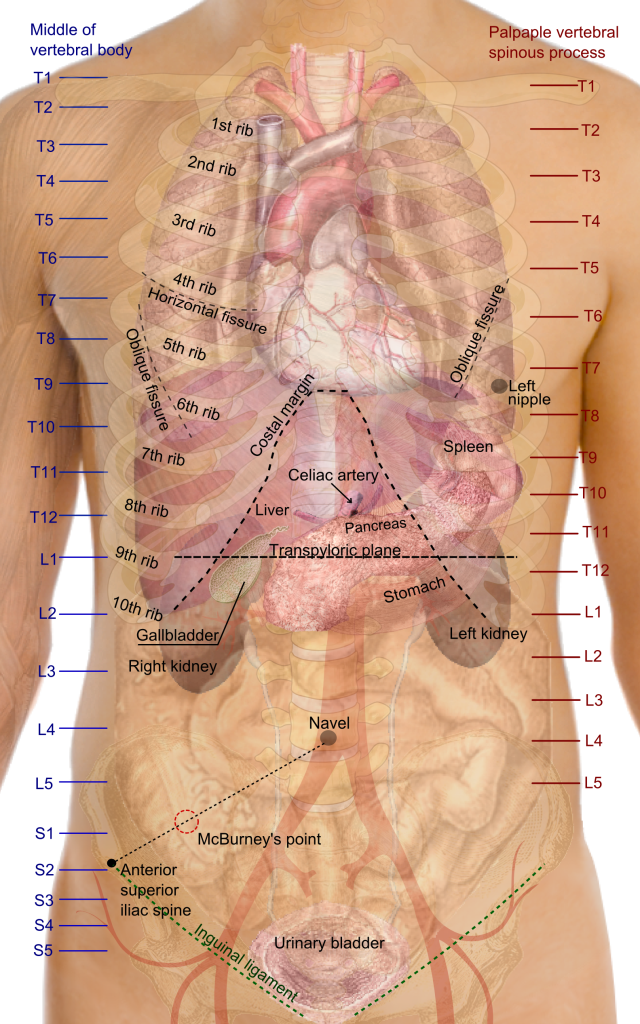
The mediastinum comprises the heart, thoracic aorta, trachea, and esophagus and is anatomically located in the center of the chest between the right and left hemithoraces. It is bordered by the sternum anteriorly, vertebral column posteriorly, and parietal pleura and lungs bilaterally and extends from the thoracic inlet superiorly to the diaphragm inferiorly. The most common isolated mediastinal injury in blunt trauma is an injury to the aorta, which can range in severity from an intimal laceration to complete aortic transection. In penetrating trauma, all the mediastinal structures are equally susceptible, and the injury sustained depends on the anatomic location of the penetrating wound and its trajectory. Of particular importance is an injury within the “cardiac box” whose boundaries are the midclavicular lines laterally, the clavicles superiorly, and the xiphoid process inferiorly. Trauma in this region is associated with an increased risk of penetrating cardiac injury and the development of cardiac tamponade, and rapid clinical decompensation.
Morbidity and mortality associated with thoracic trauma are due to the disruption of respiration, circulation, or both. Respiratory compromise can occur due to direct injury to the airway or lungs, as is the case with pulmonary contusions, or from interference in the mechanics of breathing, as with rib fractures. The common outcome is the development of ventilation-perfusion mismatch and decreased pulmonary compliance. This then results in hypoventilation and hypoxia, which may necessitate intubation. Circulatory compromise occurs in the setting of significant blood loss, decreased venous return, or direct cardiac injury. Intrathoracic bleeding most commonly manifests as hemothorax in both blunt and penetrating trauma, and a massive hemothorax can lead to hypotension and hemodynamic shock.
