Bleeding Control
Published .

Researchers have studied whether laypeople realize the severity of the situation when someone in their proximity begins to bleed, and whether they can estimate how much the person is bleeding. The results show a discrepancy related to the victim’s gender: for a woman losing blood, both blood loss and life-threatening injuries were underestimated. Despite appearances, the severity of blood loss can be assessed by the volume of blood lost, the rate at which the blood was lost, and/or age and pre-existing health of the patient (infants don’t fare as well as adults). It is important for medics to understand the factors that make bleeding worse:
- Clotting and Clotting Disorders – Patient’s with clotting disorders such as hemophilia will lose more blood than those that don’t due to an inability to produce a blood clot.
- Movement of Injured Area – Patient’s who are bleeding and start walking always leave a blood trail. Every time the patient stops, a larger pool of blood collects; when they start moving again, the pool becomes smaller. Movement not only doesn’t stop the flow of blood, it makes the patient bleed worse. For this reason, when bleeding is stopped, it is important to
- Body Temperature – In investigations of how hypothermia during surgery affects bleeding and transfusions, it was concluded that even mild hypothermia (<1°C) significantly increases blood loss by approximately 16% (4%–26%)
- Medication – Some medications decrease the body’s ability to stop bleeding. Anticoagulants like coumadin and warfarin actually prevent coagulation from occurring. Plavix and aspirin are commonly prescribed and result in platelets become less conducive to sticking together and thus, making a clot.
- Removal of Dressings – Any time blood has been stopped, a blood clot will form. If the blood clot is disturbed, it will no longer dam flow of blood and the patient’s bleeding will continue. Removing bandages or dressings from a bleeding wound will rip the clot apart and cause the bleeding to return. If a dressing becomes soaked with blood, simply cover the dressings with more dressings and continue applying direct pressure.
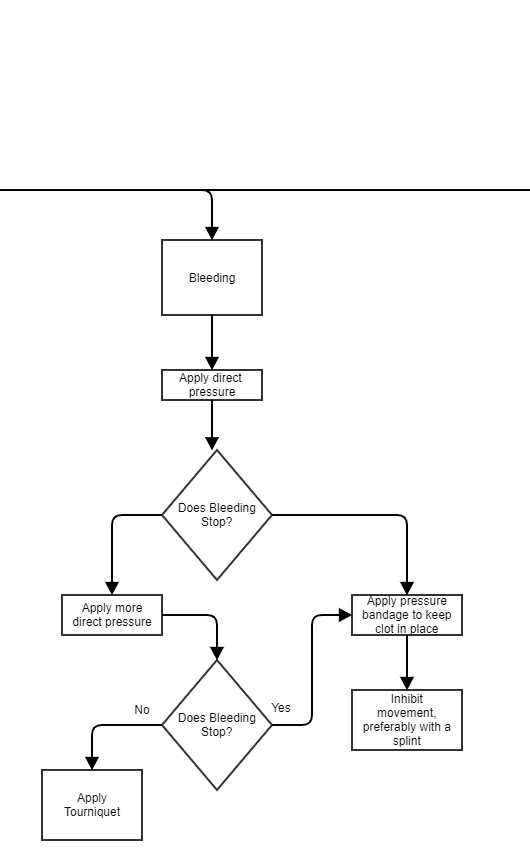
Direct Pressure Makes A Clot
The application of direct pressure with a gloved hand or a glove hand with dressings will result in a cessation of blood flow through the wound and eventually make a blood clot. This process is called hemostasis. How much pressure should be applied is often the question. Firm is the word used to describe the amount of force that should be applied to the wound. If the bleeding is soaking the dressing, simply pile on more dressings on top of the soiled dressings and continue the application of firm pressure. Firm pressure should be continually applied, for as long as 10 minutes. It may be necessary to continue applying firm pressure during transport.

Once the bleeding has been controlled, the clot should be secured with a pressure bandage. If possible, splint the extremity. If the bleeding was to the torso, consider placing the patient onto a long backboard to inhibit movement which will keep the clot in place.
Tourniquets Stop The Flow Of Blood So The Wound Doesn’t Bleed
If the bleeding won’t stop or even slow down with direct pressure, it’s time for a tourniquet. A tourniquet cuts off the blood supply so the wound doesn’t bleed. Tourniquets have two downsides. For one the extremity will no longer have a blood supply which may result in long term damage or even amputation. The second downside is the tourniquet is extremely painful to the patient. The tourniquet is applied 2 inches over the wound and not over a joint (as compressing the joint will not compress the blood vessel). If the tourniquet fails to stop the bleeding, a second tourniquet can be applied 2 inches above the first tourniquet. The tourniquet is considered a last ditch effort for bleeding control as it is seen as better than bleeding to death.
Assessment & Management Of Bleeding
Serious bleeding doesn’t just happen and is often the result of a significant mechanism of injury. The presence of a significant mechanism of injury should result in the medics eventually looking for injuries. Initial management of the patient is always guided by the primary survey. The source of the bleeding must be located. For this, the medics may need to perform a rapid trauma assessment to fully expose the patient and locate the source of bleeding. Once the source of bleeding has been found, the medics should stop the bleeding with direct pressure.
Estimating the amount of blood loss can be challenging, but the very first thing the physician is going to want to know is how much blood the patient has lost. Blood loss hard to gauge based on patient behavior as many patients will descend into a quiet and calm disposition. Further, the amount of blood found at the patient’s side can be misleading, especially if the patient moved from a different location. It would be well enough to say that the bleeding was significant and start looking for sign of shock.
Preventing heat loss is another necessary intervention. A patient who has lost a significant amount of blood quickly loses their ability to thermoregulate. Hypothermia associated with trauma (primarily blood loss) is associated with higher mortality and longer hospital stays. Preventing heat loss may mean more than just covering the patient with blankets. The medics could turn the heat on in the back of the ambulance and put hot packs in the groin and armpits.
Rapid transport to a capable hospital should happen as soon as possible. The patient may need to be transported to a trauma center. There is a good chance that the patient will meet the ‘Step One’ criteria if the blood loss is profound. Depending upon the bleeding wound, the patient could also meet ‘Step Two’ criteria. If the trauma center isn’t within a reasonable distance of the incident, the patient may need medical air transport (helicopter). All of these factors differ from response area to response area, therefore ambulance services should anticipate the needs of the areas they serve.
