Understanding Field Triage of Injured Patients
Published (updated: ).
The Purpose Of The Field Triage Of Injured Patients
Trauma centers provide a host of immediately available care by trained specialists around the clock. The care received by patients is of the highest quality, despite their ability to pay. Hospitals with trauma centers cannot affordably be placed in every hospital or even every region. Depending upon the distance to a trauma center, the patient may benefit from medical air transport (helicopter) to the trauma center. Due to the scarcity of the trauma center resources, EMS must be triage these patients properly. Triaging means ‘to sort’ in French’. Triaging these patients to a trauma center may require flying or making alternate transportation arrangements (especially from outlying regions). The Centers for Disease Control and Prevention issued the following guidance for EMS personnel in 2011.
Terms Used In The Document
- Blunt trauma – an injury to the body caused by forceful impact, injury, or physical attack with a dull object or surface. From the perspective of a surgeon, blunt trauma is typically harder to diagnose what internal injuries the patient has sustained. Blunt trauma can be caused by a fall, being struck by a car, or a falling object.
- Penetrating trauma – occurs when a foreign object pierces the skin and enters the body creating a wound. Penetrating trauma can further be classified as low velocity (stabbing) and high velocity (gun shot wound).
- Degloving – a traumatic injury that results in the top layers of skin and tissue being torn away from the underlying muscle, connective tissue or bone.
Understanding Step One
In Step One, the Glasgow Coma Scale, and Respiratory Rate criteria were modified. Step One is intended to allow for rapid identification of critically injured patients by assessing level of consciousness (Glasgow Coma Scale and measuring vital signs (systolic blood pressure and respiratory rate). These criteria demonstrate high predictive value for severe injury. Of 289 references identified from the structured literature review, 82 (28%) were relevant to Step One. SBP <90 and respiratory rate <10 or >29 remain significant predictors of severe injury and the need for a high level of trauma care. The Panel recommended transport to a facility that provides the highest level of care within the defined trauma system if any of the following are identified:
- Glasgow Coma Scale ≤13, or
- SBP of <90 mmHg, or
- respiratory rate of <10 or >29 breaths per minute (<20 in infant aged <1 year), or need for ventilatory support.
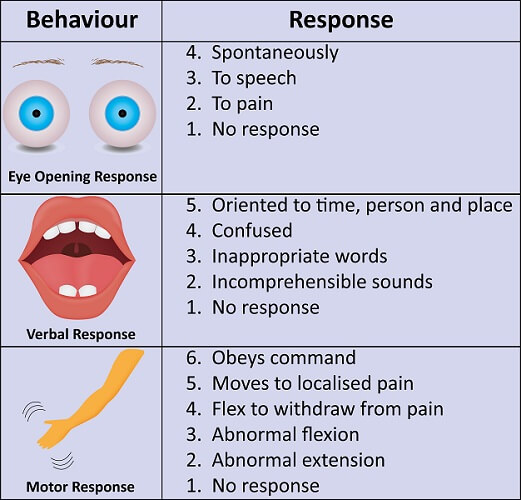
The Glasgow Coma Scale
This section discusses patients with signs of shock, altered mental status, or confusion. It mentions the Glasgow Coma Scale < 13 being a parameter for admittance under step one. The Glasgow Coma Scale was first published in 1974 at the University of Glasgow by neurosurgery professors Graham Teasdale and Bryan Jennett. The Glasgow Coma Scale (GCS) is used to objectively describe the extent of impaired consciousness in all types of acute medical and trauma patients. The scale assesses patients according to three aspects of responsiveness: eye-opening, motor, and verbal responses. Reporting each of these separately provides a clear, communicable picture of a patient’s state.
Understanding Step Two
In Step Two, the criteria pertaining to chest and extremity injuries were modified. Step Two of the Guidelines recognizes that certain patients, on initial presentation to EMS providers, have normal physiology but have an anatomic injury that might require the highest level of care within the defined trauma system.
The Panel recommended transport to a facility that provides the highest level of care within the defined trauma system if any of the following are identified:
- all penetrating injuries to head, neck, torso, and extremities proximal to elbow or knee;
- chest wall instability or deformity (e.g. flail chest);
- two or more proximal long-bone fractures;
- rushed, degloved, mangled, or pulseless extremity;
- amputation proximal to wrist or ankle;
- pelvic fractures;
- open or depressed skull fractures; or
- paralysis.
Understanding Step Three
In Step Three, the intrusion criterion was modified to include roof intrusion. An injured patient who does not meet Step One or Step Two criteria should be evaluated in terms of mechanism of injury (MOI) to determine if the injury might be severe but occult. Evaluation of MOI will help to determine if the patient should be transported to a trauma center. Although different outcomes have been used, recent studies have demonstrated the usefulness of MOI for field triage decisions. A retrospective study of approximately 1 million trauma patients indicated that using physiologic and anatomic criteria alone for triage of patients resulted in undertriage, implying that using MOI for determining trauma center need helped reduce the problem of undertriage. Another study of approximately one half million patients determined that MOI was an independent predictor of mortality and functional impairment of blunt trauma patients. The Panel recommended transport to a trauma center if any of the following are identified:
- Falls
- adults: >20 feet (one story = 10 feet)
- children: >10 feet or two to three times the height of the child
- High-risk auto crash
- intrusion, including roof: >12 inches occupant site; >18 inches any site
- ejection (partial or complete) from automobile
- death in same passenger compartment
- vehicle telemetry data consistent with a high risk for injury;
- Automobile versus pedestrian/bicyclist thrown, run over, or with significant (>20 mph) impact; or
- Motorcycle crash >20 mph
Understanding Step Four
In Step Four, the criteria for older adults and anticoagulation were modified, and the criteria for end stage renal disease requiring dialysis and time-sensitive extremity injury were removed. In Step Four, EMS personnel must determine whether persons who have not met physiologic, anatomic, or mechanism steps have underlying conditions or comorbid factors that place them at higher risk of injury or that aid in identifying the seriously injured patient. Persons who meet Step Four criteria might require trauma center care. A retrospective study of approximately 1 million trauma patients indicated that using physiologic and anatomic criteria alone for triage of patients resulted in a high degree of under triage, implying that using special considerations for determining trauma center need helped reduce the problem of under triage. The Panel recommended transport to a trauma center or hospital capable of timely and thorough evaluation and initial management of potentially serious injuries for patients who meet the following criteria:
- Older adults
- risk for injury/death increases after age 55 years
- SBP <110 might represent shock after age 65 years
- low impact mechanisms (e.g., ground-level falls) might result in severe injury
- Children
- should be triaged preferentially to pediatric capable trauma centers
- Anticoagulants and bleeding disorders
- patients with head injury are at high risk for rapid deterioration
- Burns
- without other trauma mechanism: triage to burn facility
- with trauma mechanism: triage to trauma center
- Pregnancy >20 weeks
- EMS provider judgment
