Pulmonary Edema
Published .
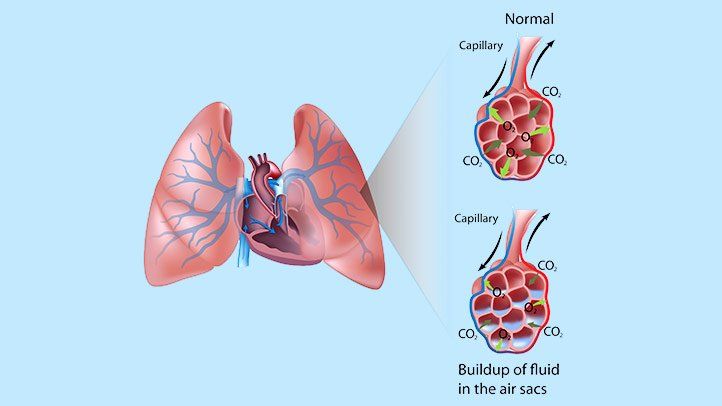
High Blood Pressures In The Pulmonary Capillaries Decreases Diffusion Of Oxygen From The Environment
Pulmonary edema is an abnormal buildup of fluid in the lungs. This buildup of fluid leads to shortness of breath. Pulmonary edema is often caused by congestive heart failure. When the heart is not able to pump efficiently, blood can back up into the veins that take blood through the lungs. Congestive heart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptoms to occur throughout the body. As the pressure in these blood vessels increases, fluid is pushed into the air spaces (alveoli) in the lungs. This fluid reduces normal oxygen movement through the lungs. These two factors combine to cause shortness of breath. Congestive heart failure that leads to pulmonary edema may be caused by:
- Heart attack, or any disease of the heart that weakens or stiffens the heart muscle (cardiomyopathy)
- Leaking or narrowed heart valves (mitral or aortic valves)
- Sudden, severe high blood pressure (hypertension)
Pulmonary edema may also be caused by:
- Certain medicines – Namely narcotics but nobody can figure out why
- High altitude exposure – High altitude pulmonary edema (HAPE) occurs during exposure to the low air pressure found at high altitudes. The normal blood pressure at sea level in the pulmonary capillaries is too high to keep blood products from leaking out of the tiny blood vessels when the air pressure drops. Air pressure decreases as altitude increases. These symptoms seem to appear at 8200 feet. Aircraft are pressurized to keep the passengers from experiencing the loss of air pressure as the aircraft climbs to that 30,000 feet.
- Kidney failure – The kidneys are no longer filtering out the fluids in the blood. This condition leaves the patient with a massive fluid overload. It’s always the worst before dialysis (at 4AM).
- Narrowed arteries that bring blood to the kidneys – Decreased blood flow to the kidneys mean the kidneys will filter less blood and remove less fluid.
- Lung damage caused by poisonous gas or severe infection –
- Major injury
Symptoms
Symptoms of pulmonary edema may include:
- Coughing up blood or bloody froth
- Difficulty breathing when lying down (orthopnea)
- Feeling of “air hunger” or “drowning” (This feeling is called “paroxysmal nocturnal dyspnea” if it causes you to wake up 1 to 2 hours after falling asleep and struggle to catch your breath.)
- Grunting, gurgling, or wheezing sounds with breathing
- Problems speaking in full sentences because of shortness of breath
Other symptoms may include:
- Anxiety or restlessness
- Decrease in level of alertness
- Leg or abdominal swelling
- Pale skin
- Sweating (excessive)
Focused Physical Exam
Medics will be dispatched to a patient with shortness of breath. The primary survey will require immediate administration of 15 lpm oxygen via non-rebreather mask. As the medics assess the patient with focused history and physical exam, they will typically make the following observations:
- Crackles in the lungs
- Increased heart rate (tachycardia)
- Rapid breathing (tachypnea)
- Hypertension
- Leg or abdominal swelling
- Jugular vein distention (JVD)
- Pale or blue skin color (pallor or cyanosis)
Treatment – Oxygen, CPAP, Assistive Ventilations, And Fowlers Position

The treatment for congestive heart failure or pulmonary edema is straightforward. Immediately increasing oxygen intake with a non-rebreather mask at 15lpm. When the above observations are made, the medics should administer oxygen via constant positive airway pressure mask (CPAP). CPAP will increase the pressure inside the chest and increase oxygen diffusion. Additionally, the patient’s blood pressure will drop due to the increase in intra-thoracic pressure caused by the CPAP. In the event that the patient cannot tolerate CPAP, oxygen should be administered via non-rebreather mask. If the patient deteriorates while enroute (the patient is struggling for air or has altered mental status), the medics can assist ventilations with a bag valve mask while the patient is sitting upright on the stretcher. Many medics make the move to lower the patient when the patient decompensates only to be rewarded with the patient becoming apneic and pulseless.
- Oxygen is given through a face mask or tiny plastic tubes are placed in the nose.
- A breathing tube may be placed into the windpipe (trachea) so you can be connected to a breathing machine (ventilator) if you cannot breathe well on your own.
