Management of Toxicological Emergencies
Published .
When EMS are dispatched to a toxicological emergency, the importance of the scene size up cannot be underestimated. Much of the scene size up can be performed while enroute to the scene. If the call was made as a suicide attempt, the medics should ensure police are enroute as well. Suicidal patients sometimes attack ambulance crews. If the location is an industrial site, the fire department needs to be enroute as well in the event the patient needs to be decontaminated or the spill needs to be contained. The ambulance could have been requested by the police. The ambulance could have been requested by a frantic mother who has discovered her child has eaten a handful of her medications. Sometimes the call is so vague that the medics have to listen to the dispatcher and connect the dots. Multiple patient’s complaining of shortness of breath should make the medics consider the possibility of carbon monoxide or other toxic gas.
Initial management of the patient is guided by the primary survey. Taking patient assessment one step at a time will ensure that the patient’s immediate needs for airway control and breathing are met. In the case of an exposure to an industrial chemical, the patient may need to be decontaminated prior to transport. All toxicological emergencies benefit from contacting poison control (800.222.1222) prior to transport is a great way to ensure the patient is decontaminated and transported to the most appropriate hospital.
Don’t Forget To Contact Medical Control
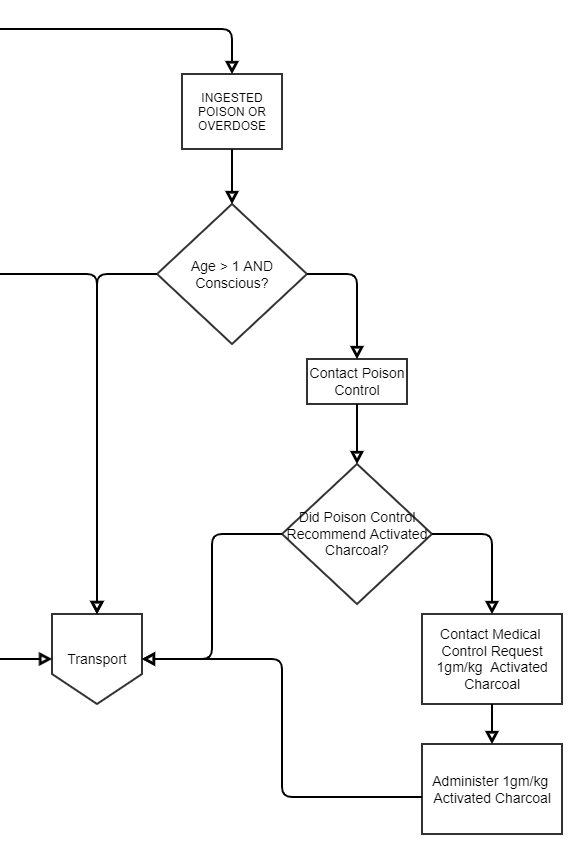
Depending upon the substance, poison control may advise EMS to administer activated charcoal. Medics should be warned that advice from poison control is just that, advice. Orders for any drug need to come through medical control. After speaking with poison control, the medics should request orders for activated charcoal from the physician at the emergency department.
Activated charcoal has pores that can trap chemicals. It is typically taken by mouth as a treatment for some swallowed poisons. There is little evidence for other uses. Charcoal is made from peat, coal, wood, coconut shell, or petroleum. Activated charcoal is made by heating charcoal in the presence of a gas. This process causes the charcoal to develop lots of internal spaces or pores. These pores help activated charcoal trap chemicals. Activated charcoal is commonly used to treat poisoning. It is also used for high cholesterol, hangovers, and upset stomach, but there is no strong scientific evidence to support most of these uses.

Contraindications
- Patients with an unprotected airway (in other words, a depressed level of consciousness) without endotracheal intubation
- If activated charcoal use is likely to increase the risk and severity of aspiration of a toxin (hydrocarbons with high aspiration potentials)
- When activated charcoal is known to not meaningfully adsorb the ingested toxin such as metals, acids, alkalis, electrolytes, or alcohols
Administration
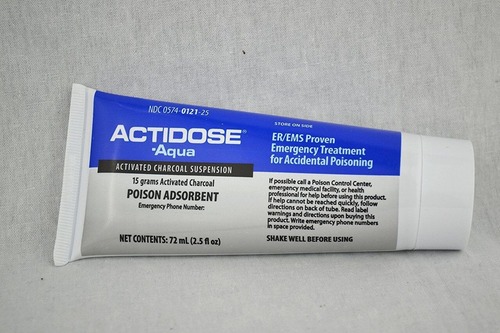
Medics should administer activated charcoal when they believe an ingested toxin is still in the gastrointestinal tract and when the benefits of preventing the absorption of the toxin are assumed to outweigh the risks posed by administering activated charcoal. The optimal dosing of activated charcoal is unknown. Activated charcoal administration can be oral or via nasogastric and orogastric tubes. When the amount of toxin ingested is unknown, activated charcoal should be administered at a dose of 1 g/kg of body weight.
