Perfusion – It’s All About The Flow
Published .

Perfusion is the passage of fluid through the circulatory system or lymphatic system to an organ or a tissue, usually referring to the delivery of blood to a capillary bed in tissue. Perfusion is measured as the rate at which blood is delivered to tissue, or volume of blood per unit time (blood flow) per unit tissue mass. The word is derived from the French verb “perfuser” meaning to “pour over or through”. All animal tissues require an adequate blood supply for health and life. Poor perfusion (hypoperfusion), that is, ischemia, causes health problems, as seen in cardiovascular disease, including coronary artery disease, cerebrovascular disease, peripheral artery disease, and many other conditions.
Perfusion pressure is how much pressure it takes to push blood through all the blood vessels in a specific area. As long as this pressure is high enough, blood will continue to flow through those vessels. That means that perfusion pressure is a critical part of how your body’s circulatory system works.
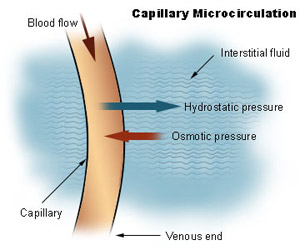
When perfusion pressure in certain areas drops too low, that can lead to major problems. The two most vulnerable areas where this can happen the heart and brain. When either of these organs isn’t getting enough blood flow, it can lead to serious or life-threatening conditions. The heart’s pumping action constantly pushes blood throughout the body, with every heartbeat propelling blood out of the heart and into arteries. Blood then flows from the arteries and to the capillaries, where the blood delivers oxygen to cells. Once that part of the job is complete, the blood in the capillaries enters the veins and returns to your heart. This cycle repeats with every heartbeat.
Perfusion is about flow, which is related to a host of factors, including circulatory volume, peripheral resistance, and cardiac output. Cardiac output (CO) is the amount of blood pumped by the heart minute and is the mechanism whereby blood flows around the body, especially providing blood flow to the brain and other vital organs. The body’s demand for oxygen changes, such as during exercise, and the cardiac output is altered by changing both heart rate (HR) and stroke volume (SV). As a result, the regulation of cardiac output is subject to a complex mechanism involving the autonomic nervous system, endocrine, and paracrine signaling pathways.
Blood Flow Makes It Possible For Cells To Breath
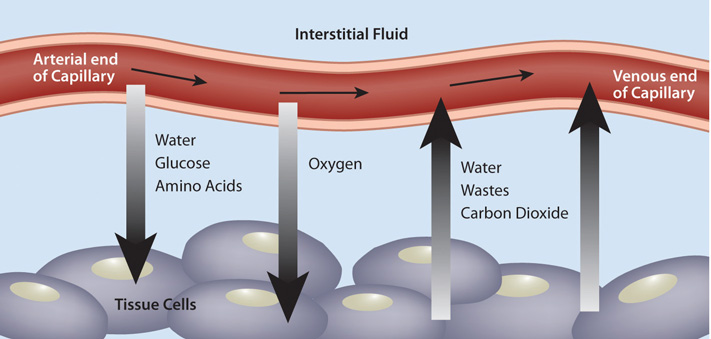
Red blood cells carry the oxygen into the capillaries of the tissues of the body. Oxygen diffuses into the cells of the tissues, while carbon dioxide (the waste product of aerobic metabolism) diffuses out of the cells of the tissues and into the bloodstream.
The factors that influence tissue gas exchange are similar to the factors of alveolar gas exchange, and include partial pressure gradients between the blood and the tissues, the blood perfusion of those tissues, and the surface areas of those tissues. Each of those factors generally increase gas exchange as those factors are increased (i.e., more oxygen diffusion in tissues with more blood perfusion).
Inadequate Blood Flow Suffocates Cells
Inadequate blood perfusion (flow) leads to problems with oxygen delivery to cells. Without the constant supply of oxygen, the cells will not receive oxygen. The cells won’t immediately die, but without oxygen it’s just a matter of time before cells start dying. When the conditions are ripe for massive cell death, the body starts making some moves to increase perfusion in the patient’s core. This movement of blood from the patient’s extremities into the core is what results in the tried and true symptoms of shock (weak radial pulse, tachycardia, hypotension, tachypnea). The following conditions would result in decreased blood flow or hypoperfusion:
- Tachycardia – Various conditions can result in the patient’s heart beating too fast for their needs. Since the heart fills during diastole (between heartbeats), a rapid heart rate will result in decreased diastolic filling time. Less blood coming in means less blood going out.
- Bradycardia – Various conditions can result in the patient’s heart beating too slow for their needs. If the stroke volume (the amount of blood ejected with each heartbeat) remains the same, but the rate decreases, less blood will leave the heart every minute.
- Pump – If heart fails to pump all of the blood out of the ventricles (whether right or left) or ejects the blood at a pressure that is insufficient to create the ‘wave’ of blood flow required to get to furthest reaches of the circulatory system, the result will be less flow or perfusion.
- Volume – If the circulating volume drops due to blood loss or blood pooling, the result will be hypovolemia (low blood volume). Decreased blood volume will result in decreased flow or perfusion and less cardiac output.
- Vasodilation – If all the great vessels of the body suddenly became twice as large as they normally are, the result would be decreased blood flow due to a lack of peripheral vascular resistance. Various mechanism result in vasodilation; including anaphylaxis, sepsis, and neurogenic shock.
