Acute Coronary Syndrome
Published .
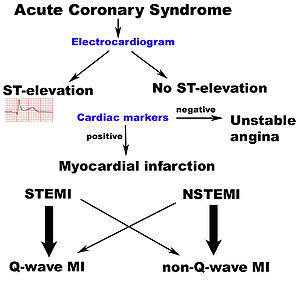
Acute coronary syndrome (ACS) refers to a group of conditions that include ST-elevation myocardial infarction (STEMI), non-ST elevation myocardial infarction (NSTEMI), and unstable angina. It is a type of coronary heart disease (CHD), which is responsible for one-third of total deaths in people older than 35. Some forms of coronary heart disease can be asymptomatic, but Acute coronary syndrome is always symptomatic.
Etiology
ACS is a manifestation of CHD (coronary heart disease) and usually a result of plaque disruption in coronary arteries (atherosclerosis). The common risk factors for the disease are smoking, hypertension, diabetes, hyperlipidemia, male sex, physical inactivity, family obesity, and poor nutritional practices. Cocaine abuse can also lead to vasospasm. A family history of early myocardial infarction (55 years of age) is also a high-risk factor.
Epidemiology
CHD affects about 15.5 million in the United States. The American Heart Association estimates a person has a heart attack every 41 seconds. Heart disease is the leading cause of death in the United States. Chest pain is among the top reasons for emergency department visits.
Pathophysiology
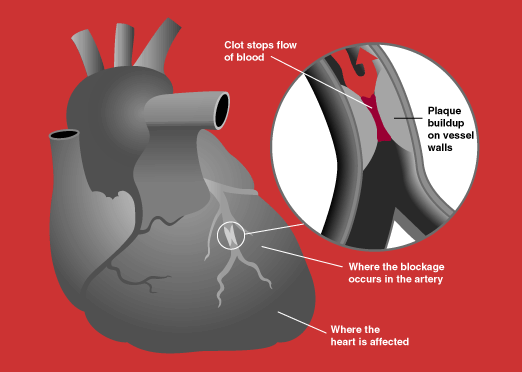
The underlying pathophysiology in ACS is decreased blood flow to part of heart musculature which is usually secondary to plaque rupture and formation of thrombus (clot). Sometimes ACS can be secondary to vasospasm with or without underlying atherosclerosis. The result is decreased blood flow to a part of heart musculature resulting first in ischemia and then infarction of that part of the heart.
History and Physical
The classic symptom of ACS is substernal chest pain, often described as crushing or pressure-like feeling, radiating to the jaw and/or left arm. This classic presentation is not always seen, and the presenting complaint can be very vague and subtle with chief complaints often being difficulty breathing, lightheadedness, isolated jaw or left arm pain, nausea, epigastric pain, diaphoresis, and weakness. Female gender, patients with diabetes, and older age are all associated with ACS presenting with vague symptoms. A high degree of suspicion is warranted in such cases. They variation of complaints with acute coronary syndrome can be enormous, medics should suspect acute coronary syndrome when during the interview the patient confides a history of the following complaints:
- Shortness of breath (dyspnea) – The dyspnea could be continuous, exertional, non-exertional, orthopneic
- Cough – the cough could be dry or productive
- Nausea
- Vomiting
- Palpitations (heart fluttering)
- Headache
- Recent trauma
As a general rule, patients with chest pain are experiencing acute coronary syndrome. Dispatchers typically send an ALS response to chest pain. The Paramedics will assess the patient, perform a 12 lead EKG, and pre-treat the patient for the Cath lab. Nonetheless, the index of suspicion for acute coronary syndrome should be increased when the following history is obtained from the patient:
- Angina – a condition marked by severe pain in the chest, often also spreading to the shoulders, arms, and neck, caused by an inadequate blood supply to the heart.
- Previous AMI (acute myocardial infarction or heart attack)
- Hypertension
- Heart Failure
- Valve disease
- Aneurysm
- Pulmonary disease
- COPD
- Renal Disease
In the physical exam, general distress and diaphoresis are often seen. Heart sounds are frequently normal. At times, gallop and murmur can be heard. Lung exam is normal, although at times crackles may be heard pointing toward associated congestive heart failure (CHF). Bilateral leg edema may be present indicating CHF. The rest of the systems are typically within normal limits unless co-pathologies are present. The presence of abdominal tenderness to palpation should make the provider consider other pathologies like pancreatitis and gastritis. The presence of unequal pulses warrants consideration of aortic dissection. The presence of unilateral leg swelling should warrant work-up for pulmonary emboli. Hence a thorough physical exam is very important to rule out other life-threatening differentials.
