Psychiatric
Published (updated: ).

Behavior is the way in which someone conducts oneself or behaves. A psychiatric disorder or mental disorders (or mental illnesses) are conditions that affect thinking, feeling, mood, and behavior. They may be occasional or long-lasting (chronic). A behavioral emergency is defined as a situation in which a patient presents as being at imminent risk of behaving in a way that could result in serious harm or death to self or others.
Ambulances are dispatched to behavioral emergencies everyday. Often, the ambulance is requested by police who are responding to a disturbance. Sometimes, the police are quick to determine the patient needs an ambulance, other times not. Prior to the arrival of the ambulance, the situation often becomes heated, resulting in a situation that may be more volatile than the medics are comfortable with. The medics need to understand that they are there to help the patient and serve a different role than the police. This is a good time for the medics to act like medics and not try to act like police.
The Ways Of The Medic
Medics shouldn’t expect a normal encounter with a patient experiencing a behavioral emergency. The patient could be violent, uncooperative, or very cooperative and forthcoming. In short, they are not all the same. It helps to establish some rapport with the patient, and the easiest way to do that is try to treat the patient like any other patient. Patients with psychiatric disorders are well versed in the medical interview process. The familiar process is likely to be well received by the patient.
Not all psychiatric patients are violent. It is easy to spot the ones that are violent; predicting violence for the most part is easy. The medics have to consider the possibility that the patient will continue being violent in the back of the ambulance. The ambulance is no place for a violent confrontation because the medic always loses (either getting hurt, dead, or defending and hurting the patient). If the prediction of violence in the ambulance can be made, it’s time to contact medical control and request orders to restrain and transport the patient against their will.
Acute Psychosis
Psychosis is a condition characterized by loss of contact with reality and may involve severe disturbances in perception, cognition, behavior, and feeling. Approximately 3% of people will experience a psychotic episode at some stage in their life. Usually a person’s first episode occurs in adolescence or early adult life, an important time for the development of identity, relationships and long-term vocational plans. The initial episode of psychotic disorders can be particularly confusing and traumatic for the person and their family. A lack of understanding of psychosis often leads to delays in seeking help. As a result, these treatable illnesses are left unrecognized and untreated. Even when appropriate help seeking does occur, further delays in diagnosis and treatment may result from skill and knowledge gaps among professionals. Increasingly, attention is being paid to strategies that reduce the personal, social and economic strain of these conditions on affected individuals, their families and the community. Early intervention in first-episode psychosis is aimed at shortening the course and decreasing the severity of the initial psychotic episode, thereby minimizing the many complications that can arise from untreated psychosis. It is a strategy that can provide considerable long-term benefits.
Agitated Delirium
Excited (or agitated) delirium is characterized by agitation, aggression, acute distress and sudden death, often in the pre-hospital care setting. It is typically associated with the use of drugs that alter dopamine processing, hyperthermia, and, most notably, sometimes with death of the affected person in the custody of law enforcement. Subjects typically die from cardiopulmonary arrest, although the cause is debated. Unfortunately an adequate treatment plan has yet to be established, in part due to the fact that most patients die before hospital arrival.
The agitated delirium patient encounter is generally initiated by police, who have responded to some sort of disturbance, therefore it’s likely that the scene will be safe and the patient searched for weapons. The police would consider arresting the patient, however on what charges? This is why police call EMS. As stated above, establish a rapport with the patient by initiating the SAMPLE history conversation and try to listen to what the patient says (and write it down). The patient will probably not appreciate any unnecessary touching, so the medics should ensure that the patient is forewarned of any encroachment into their space.
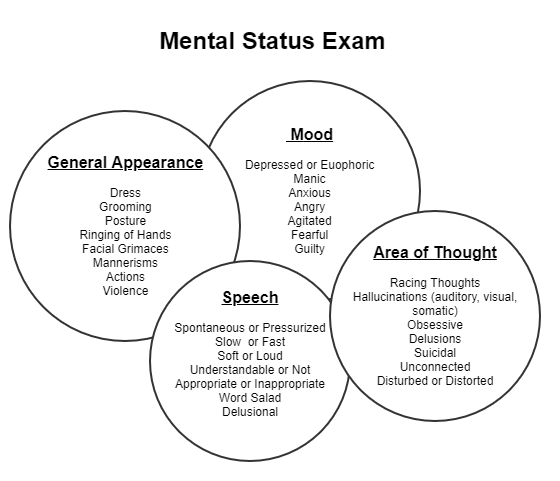
Assuming the patient is communicating with the medics, they could try the mental status examination. Assess the following
- Level of Consciousness – The patient will be alert, otherwise the medics wouldn’t really be interested in performing the mental status examination.
- General Appearance – Clean or dirty, clothing or lack thereof
- Speech & Motor Activity – Assess the patient speech for slurring, dysarthria. Assessing motor activity can be accomplished by asking the patient to follow some commands. Consider pulse, motor, sensory perception and the Cincinnati Prehospital Stroke Scale.
- Attitude & Insight – Does the patient seem to have a positive or negative attitude. What does the patient think is going to happen next?
Management

